Heading Title
As you may know by now, cancer is not always a death sentence. Due to the complexity and uncertainty of it all, we have a lot of fear and those fears are often exacerbated by erroneous information. When it comes to “The Big C”, there are a lot of myths and misconceptions out there. Today, I have identified and broken down 6 common myths about cancer.
Myth # 1: Using artificial sweeteners causes cancer?

This is false and numerous studies have found no evidence that: Sweet ‘N Low; Equal, NutraSweet; Sweet One and Splenda causes cancer in humans. All of these sugar substitutes, except for Equal, have been approved by the Food and Drug Administration for consumption in the United States. So, the next time you want to reach for Sweet ‘N Low or Splenda to sweeten your coffee and tea, you can do so with ease. I, however, have never been a fan of the artificial sweeteners. I’m an addict and crave the real thing. In the words of Chris Rock aka Pookie from the movie, New Jack City “It keeps calling me.” No worries, I’m getting help for it(LOL).
Myth # 2: Having a positive outlook will reduce my chances of acquiring cancer and/or cure cancer.

There is some truth to this, but it isn’t a simple true or false question. A 2014 study from the American Journal of Epidemiology considered the incidence of cancer in women measuring stress levels for five years prior to diagnosis and found no definite proof between stress level and the diagnosis of cancer. Therefore, it is inconclusive whether stress directly leads to an increased chance of developing cancer. However, there have been other studies demonstrating a correlation between lowered stress levels and improvement in cancer patients. Having a positive outlook before and during your cancer treatments can enhance your push to remain active with loved ones, support groups, and continue with social activities- all of which are important factors in recovery.
Myth # 3: Routine checkups will lead to early detection of cancer?

It is true that regular checkups with your primary physician is a great way to note early cancer diagnoses. However, there’s no guarantee. Cancer is a complex disease, and there’s no sure way to always spot it. Routine screening has been linked to a decrease in deaths from cancers of the cervix, breast, colon and rectum. Recently, I reviewed a case where a patient was diagnosed with lung cancer, incidentally. The patient fell and broke his shoulder bone and needed imaging done for additional treatment. Through this imaging, a mass was seen and the patient was diagnosed with lung cancer. Prior to his fall, he had no complaints of symptoms relating to his cancer such as: chest pains, abnormal coughs with blood, or shortness of breath. He didn’t have a history of smoking. A routine check-up, with a primary care physician, would not have likely detected lung cancer in an asymptomatic patient. Treatment for the accidental fall, on the other hand, definitely played a major part in early detection.
Myth #4: Using my cell phone will cause cancer?

No, no, and no! Cancer is caused by genetic mutations. While cell phones do generate a type of low-frequency energy, there is no evidence that they damage genes. If cell phones really caused cancer, there would be some widely known invention in the marketplace being peddled to consumers that alleges to makes cell phone use safer (other than Bluetooth and headphones). The timeless ear-to-phone method of taking a call would not only be considered old-fashioned, but it would be obsolete.
Myth # 5: Cancer is caused by family genetics?

Cancer is caused by mutations in genes and about 10 percent of those cancers are inherited from your parents. The remaining percentage of cancers are caused by genetic changes that occur throughout a person’s lifetime as a NATURAL result of aging and exposure to environmental factors, such as tobacco smoke and radiation. The types of food you consume and your activity level may also influence your risk of being diagnosed with cancer.
Myth # 6: Dyeing your hair increases you risk of cancer?

There is no evidence that links personal hair dye use to increased risks of cancer, but hairstylist beware! Some studies suggest that hairdressers and barbers who are regularly exposed to large quantities of hair dye and other chemical products may have an increased risk of bladder cancer. This is actually news to me, and I feel compelled to share this information with my hairstylist, pronto! Who will you share this information with?
There is a lot of bad information lurking around about cancer. Now that you have the facts, I hope some of your worries are eliminated and that you will take an opportunity to learn more about cancer.
To find more information on topics mentioned above, please visit links provided below.
National Cancer Institute; www.cancer.gov
http://aje.oxfordjournals.org/content/157/5/415.long
http://www.ncbi.nlm.nih.gov/pubmed/20639214
Gago-Dominguez M, Castelao JE, Yuan JM, Yu MC, Ross RK. Use of permanent hair dyes and bladder-cancer risk. International Journal of Cancer 2001; 91(4):575–579
During your chemotherapy treatment, you may have a poor appetite or not feel up to eating. But you should try and eat what you can because good nutrition can help give your body the strength it needs to repair itself. It is also important to drink plenty of fluids throughout the day to stay hydrated.
Because your cancer and chemotherapy may make it harder for your body to fight off infections, it is good practice to follow proper food preparation and handling techniques. Most people follow these anyway, but they are really important at this time.
There are a number of things that can be done in the kitchen to lower your chances of getting sick from the food that you eat:
- Wash your hands with soap and water before handling food.
- Clean your countertops with a disinfectant, such as Lysol®.
- Rinse fruits and vegetables well to remove any germs, and peel them if necessary.
- Prepare raw meat and vegetables on different cooling surfaces.
- Thaw meat in the microwave or refrigerator.
- Clean any surfaces that you used to prepare meat well.
- Cook meat and eggs all the way through to kill any germs.
- Refrigerate leftovers promptly to prevent germs from growing.
- Eat refrigerated leftovers within 24 hours of preparation.
This article originally appeared on preventcancerinfection.org
Do you ever experience a painful, burning sensation in your chest, especially after eating certain foods? If so, it may be heartburn caused by acid reflux, which occurs when acid from your stomach backs up into your esophagus. Most of us experience heartburn occasionally, and it’s generally not a serious concern.
However, persistent acid reflux, or gastroesophageal reflux disease (GERD), can irritate the lining of the esophagus and perhaps the tissues of other respiratory and digestive organs. Over time, GERD may increase your risk of certain cancers.
“The stomach is immune to the effects of acid because it has a special lining,” explains Baran Sumer, M.D., associate professor with the Simmons Cancer Center at UT Southwestern, in a telephone interview with HealthCentral.
However, the esophagus does not have that lining. The acidity of stomach acid can be very low, Dr. Sumer says — “It’s like battery acid” — and if reflux backs up from the stomach into the esophagus, it’s very irritating.
Normally, says Dr. Sumer, the gastroesophageal sphincter and cricopharyngeal muscle in the neck clench down to prevent acid from going into the esophagus.
“These mechanisms aren’t perfect, and when they don’t function properly, you can get acid reflux in the back of the throat, your pharynx, your esophagus,” Dr. Sumer says. “People experience this as heartburn.”
Reflux disease and esophageal cancer
“There is a proven association between GERD and esophageal cancer,” says Milan Amin, M.D., associate professor in the Department of Otolaryngology—Head and Neck Surgery at NYU Langone, in a telephone interview with HealthCentral. “This is well established. It’s not a huge risk, but it is a concern because it’s difficult to treat esophageal malignancies.”
Years of esophageal exposure to stomach acid can lead to Barrett’s esophagus, a disease of the lower esophagus. Barrett’s esophagus is a risk factor for adenocarcinoma of the esophagus, a type of cancer.
“Once you have Barrett’s esophagus, there’s about a 1 percent per year conversion rate to malignancy,” says Dr. Amin.
People with long-term reflux disease should be screened periodically for esophageal malignancies, he says.
Reflux disease and cancers of the head and neck
While the link between GERD and esophageal cancer is well established, the data associating GERD with head and neck cancers is less conclusive. Most studies do show an increase in head and neck cancers in people with long-term reflux disease. However, it’s a small association, and there’s no evidence there is a cause-and-effect relationship.
“If reflux disease produces cancer in the esophagus, what happens if it escapes the esophagus and gets into the throat or a portion of the lungs?” says Dr. Amin. These structures are less protected against acid and enzyme exposure. “There’s conjecture that damage in the throat all the way up to the nose from acid reflux can produce a host of diseases, both benign and malignant.”
The most recent study, published in JAMA Otolaryngology Head and Neck Surgery in December 2017, found adults 66 and older who had respiratory and neck cancers were more likely to have GERD. The strongest association was between GERD and cancer of the larynx (voice box).
“The question is: Is there a causative effect?” Dr. Amin says. “Patients with cancer tend to be smokers, be overweight, and have other medical conditions that also raise their risk for reflux. Is there a third factor that plays a role as well? Some studies have taken out these co-morbidities [co-existing conditions] and have still found an association [between GERD and head and neck cancers].”
Dr. Amin says the vast majority of head and neck malignancies are associated with tobacco use, but that’s changing, too.
“There’s been a recent trend in the last decade of more and more head and neck malignancies that are non-smoking related,” he says. “They may be related to HPV, but not all of them. These patients tend to be younger, healthier, non-smokers. We’re not sure what the cause is.”
Should you be treated if you have reflux disease?
Dr. Amin will treat patients who have reflux disease if it’s causing symptoms or if there’s a risk of another immediate health concern, but there are some risks to keep in mind.
“There’s now some about concern about treating reflux disease aggressively because treating it with PPIs [proton pump inhibitors] is now associated with all sorts of other risks,” he says.
Different studies have shown an association between PPIs and dementia, kidney disease, heart disease, stroke and decreased bone density, which increases hip fractures among women who are long-term PPI users, he says.
“We’re more careful prescribing these medications,” Dr. Amin says. “Typically, once you start these medications, patients are almost never taken off. “
Dr. Amin wonders whether these are the patients eventually developing diseases from taking too many reflux disease medications.
“We’re more cautious now,” he says.
Diet and lifestyle changes do seem to help control reflux disease. If you have heartburn, reduce your food intake before bedtime and avoid or limit certain foods, such as alcohol, chocolate, tomatoes, caffeine, and fatty foods, which are associated with reflux. Eat smaller meals earlier in the evening and don’t lie down for two to three hours after eating.
Additionally, Dr. Amin says, some people with severe reflux find relief by lifting the head of their bed. If you are a side-sleeper, he recommends sleeping on your right side for better drainage to the stomach.
“Those lifestyle changes may very well also help decrease the risk of certain head and neck tumors,” Dr. Sumer says, although “the overall risk is very small.”
Article written by Kathleen Hall and originally appeared on heatlhcentral.com
Image:Istock
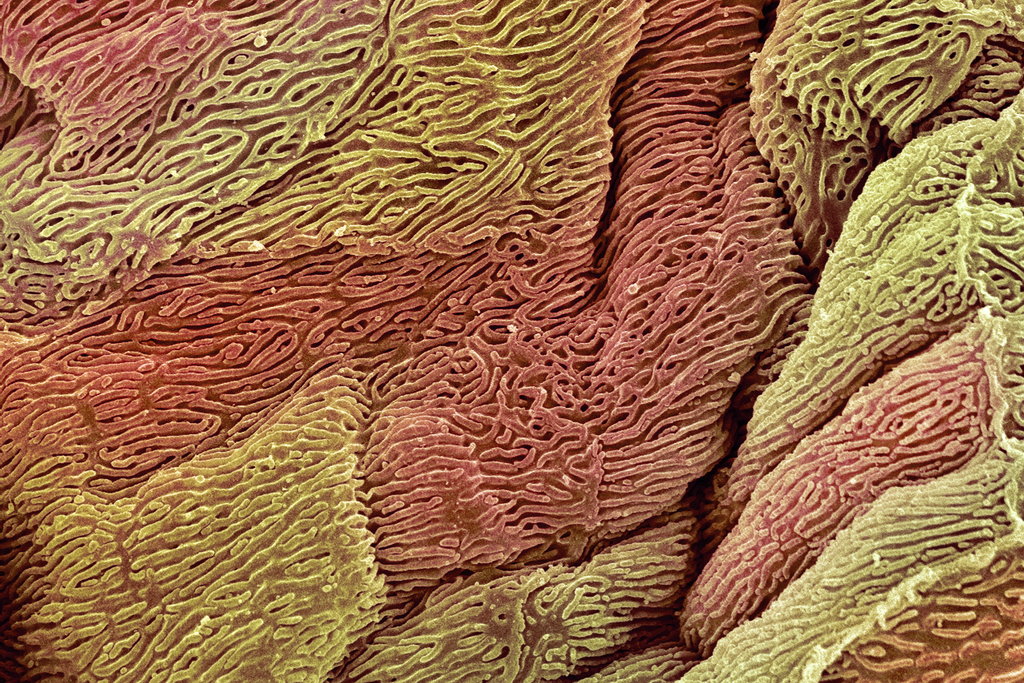
Two types of bacteria commonly found in the gut work together to fuel the growth of colon tumors, researchers reported.
Their study, published in the journal Science, describes what may be a hidden cause of colon cancer, the third most common cancer in the United States. The research also adds to growing evidence that gut bacteria modify the body’s immune system in unexpected and sometimes deadly ways.
The findings suggest that certain preventive strategies may be effective in the future, like looking for the bacteria in the colons of people getting colonoscopies.
If the microbes are present, the patients might warrant more frequent screening; eventually people at high risk for colon cancer may be vaccinated against at least one of the bacterial strains.
“I can’t guarantee you these bacteria will be the holy grail of colon cancer, but they should be high on the list” of possible culprits, said Christian Jobin, a professor of medicine at the University of Florida who studies bacteria in the gastrointestinal tract.
An estimated 50,000 Americans are expected to die of colon cancer in 2018. The new study focused on the earliest stages of the disease.
Two types of bacteria, Bacteroides fragilis and a strain of E. coli, can pierce a mucus shield that lines the colon and normally blocks invaders from entering, the researchers found. Once past the protective layer, the bacteria grow into a long, thin film, covering the intestinal lining with colonies of the microbes.
E. coli then releases a toxin that damages DNA of colon cells, while B. fragilis produces another poison that both damages DNA and inflames the cells. Together they enhance the growth of tumors.
Not everyone carries the two types of bacteria in their colon. Those who do seem to pick up microbes in childhood, where they simply become part of the diverse mass of bacteria in the intestinal tract — the so-called microbiome.
For most who carry them, it is not clear the bacteria would ever be a problem, said Dr. Eric Pamer, an infectious disease specialist at Memorial Sloan Kettering Cancer Center in New York.
The bacteria seem to be able to induce colon cancer, or to take precancerous cells and drive them faster toward cancer, said Dr. Drew Pardoll, director of Johns Hopkins’s Bloomberg-Kimmel Institute for Cancer Immunotherapy and an author of the new paper.
“Bacteria are there at the very earliest stages,” said Dr. Matthew Meyerson, director of cancer genomics at the Dana-Farber Cancer Institute in Boston. “This is a big step forward in understanding what is the role of the microbiome in colon cancer.”
The study’s lead researcher, Dr. Cynthia Sears, an infectious disease specialist at the Bloomberg-Kimmel Institute, did not expect to be investigating colon cancer.
She and her colleagues were looking at a toxin that is produced by B. fragilis. It was a familiar poison, a common cause of diarrhea.
In petri dishes, however, the toxin damages DNA and triggers cancerous changes in the epithelial cells that give rise to colon cancer. When the investigators put these toxin-secreting bacteria into mice, the animals’ colons became spotted with tumors.
So the scientists decided to investigate a broader question: Were any bacteria linked to human colon cancer and, if so, which ones?
The scientists chose to focus on two groups of patients: those who had no particular genetic risk for colon cancer but developed it anyway; and those who had a rare inherited genetic condition, familial adenomatous polyposis, or F.A.P., that almost inevitably leads to colon cancer.
In both groups, cancer begins with polyps, benign growths of colon cells that carry a mutation or two that can set them on the path to cancer. Most of the time, however, the polyps never progress and remain harmless.
But if a polyp develops a few more mutations, cancer can begin to develop. So to protect patients, doctors remove any polyps they find during a colonoscopy.
People with F.A.P. can have hundreds of polyps, their colons lined with growths. It is impossible for doctors to take them all out; instead, they may remove the patient’s entire colon.
Dr. Sears and her group examined six whole colons lined with polyps that had been removed from people with F.A.P. The researchers discovered biofilms — sheets of bacteria that had invaded the mucus covering the colons.
But the biofilms were made up of just two species of bacteria, B. fragilis and a strain of E. coli. In samples of colon tissue from healthy people, only a few had these bacteria.
The researcher also examined 25 tumor samples taken from people with F.A.P. — and found the two bacterial species again.
Then the team tried a mouse experiment, giving the animals a cancer-causing agent to elicit changes in the DNA of colon cells and then infecting them with one or the other of the bacteria. There were few or no tumors.
But when the researchers infected the animals with both types of bacteria, tumor growth took off.
The results might help explain why people with F.A.P., even individuals in the same family, can develop colon cancer at very different ages: patients who get the disease early may be carrying these two bacterial species.
Now Dr. Sears is trying to find out whether the bacteria always, or sometimes, are drivers of colon cancer in the general population.
Working with nearby community medical practices, she is examining colon tissue from every patient having a colonoscopy. She hopes to review 2,000 pathology samples.
But, she and others warn, it is premature to think of using the current results to protect people from cancer. “You could try to eliminate the bugs,” Dr. Jobin said. “That is easy to say, but hard to do. Antibiotics will probably do more damage than good.”
The drugs kill a wide variety of bacteria in gut, he added, many of which are needed for health.
The bacteria described in the new study are not the first implicated in colon cancer. Researchers have discovered a different type, fusobacteria, in more advanced colon cancer. In a recent study they reported that fusobacteria had burrowed into tumors and stayed with them as they spread throughout the body.
Article written by Gina Kolata and originally appeared on nytimes.com
Image:Pixabay
When someone is diagnosed with a vicious disease such as cancer, most people go into shock mode or become emotional and some enter depression. Being a cancer specialist who deals with cancer diagnosis on a daily, I too still feel a bit emotional when hearing the news of a loved one or patient whom I have no personal ties with. The question still remains; how does one move on during and after a cancer diagnosis?
As a professional I could say based on the stats of that particular cancer type and its’ stage, they may or may not be “OK” and prepare them for what’s ahead. Or on the other hand from a personal stand point, having dealt with multiple cancer diagnosis in my family; it’s a much tougher pill to swallow. You really have to take everything one day at a time, despite what the statistics report.
After a person falls ill we tend to think “awe poor fella, hope they feel better” and or rush to their aid, but there’s another thing we must remember and that is the well being of their caretaker. I’m aware of the major issues a cancer patient maybe dealing with many wouldn’t understand, so is the caregiver physically and emotionally. Depending on the situation a caretaker could be anyone from a spouse to significant other, child, cousin, sibling, friend or professional caretaker.
I remember some years back; one of my uncles was diagnosed with Multiple Myeloma, a cancer that affects blood plasma cells in the bone. I went to visit him and my aunt for the weekend. He wasn’t able to walk a lot on his own so, he used a walker to help him get around. I brought a few board games just to take his mind off the pain temporarily. We even played a few rounds of Bid Whist, my aunt taught me how to play while I was there. As the time passed, I sat my aunt down and ask how she was doing being that she’s my uncle primary caregiver. She paused for a moment and replied “You’re the first person to ever ask me that and I appreciate that you’re concerned with my feelings & well being.”
I mentioned that story because often times we forget that caretakers are having a rough time as well. From traveling back and forth with their loved ones to appointments, to getting them dressed, preparing meals, helping them to the bathroom, missing work, paying the bills, making sure they have proper insurance coverage. I mean, who wants to see their loved one suffering with the lost of their hair, lost feeling in their fingers/toes and constant weakness?
The list of concerns that a caregiver deals with on a daily goes on and on. I will discuss more of them in detail at a later date.
I don’t feel that its intentional behavior, but we sometimes over look them for various reasons. A cancer diagnosis doesn’t affect just that person, but everyone in their circle.
It only takes a few seconds out of your day to pick up the phone or send a text message with a cute emoji attached or even mail a “thinking of you’” card. I’m not asking or suggesting that we put our lives on hold, but to show them they are important as well. I promise you that small jester will go a long way in that individual’s mind body and soul.
We must remind them that they are not in this battle alone. WE too are here, care and ready to fight!
World Cancer Day is not just something you post with a hash tag and then move on, its a day where people all over the world should come together and focus on the seriousness of this disease, CANCER. Yes, I KNOW it’s a very tough discussion many like to over look, but it’s definitely needed! As a cancer research professional and to have experienced many cancer diagnoses personally and professionally that have affected me in ways one couldn’t’ imagine, I understand from both angles how important awareness and action really is.
Currently 8.8million (more than New York City’s population in 2016) people die from cancer worldwide every year, out of which, 4 million people die prematurely (aged 30 to 69 years).
On this day, February 4th, I challenge EVERYONE to change something they are doing that may increase their risk of cancer. For me, I’ve decided to change my eating habits and incorporate more exercising. This journey hasn’t been easy as I love sweets: cookies, cakes doughnuts, Snicker bars and for some reason I’ve started eating potato chips more often (think I need to research this). You know the saying “Rome wasn’t built in a day?” I tell myself this constantly. Also have “the talk” with your loved ones. Let’s not take the simple things for granted. Check your boobies (male & female), that month long cough, rash on your inner thigh or those abdominal pains that you brush off as cramps/gas or that old wound that seems like it doesn’t want to heal. It’s the little things we take for granted that could turn into something much bigger. Let’s pay attention to our bodies, ASK questions, and check on one another and most importantly WE are all in this TOGETHER!! This isn’t a game; it’s your life!
Below are a few preventive measures one could take in lowering their risk of cancer:
- Change diet: reduce fatty foods, limit your sugar in take (VERY hard for me), eat more green vegetables and fruit
- Implement a workout routine: daily 15-30 minute walk, running or bike riding
- Quit smoking
- Avoid Tanning beds and long periods of time with direct sunlight without proper sunscreen
- Reduce alcohol intake
“You beat cancer, by how you live, why you live and the manner in which you live.”- Stuart Scott
Image:Pixabay
Healthy cells carry a surprising number of cancer-linked mutations, but they don’t turn into tumors. What’s holding them back?
Cancer is a disease of mutations. Tumor cells are riddled with genetic mutations not found in healthy cells. Scientists estimate that it takes five to 10 key mutations for a healthy cell to become cancerous.
Some of these mutations can be caused by assaults from the environment, such as ultraviolet rays and cigarette smoke. Others arise from harmful molecules produced by the cells themselves. In recent years, researchers have begun taking a closer look at these mutations, to try to understand how they arise in healthy cells, and what causes these cells to later erupt into full-blown cancer.
The research has produced some major surprises. For instance, it turns out that a large portion of the cells in healthy people carry far more mutations than expected, including some mutations thought to be the prime drivers of cancer. These mutations make a cell grow faster than others, raising the question of why full-blown cancer isn’t far more common.
“This is quite a fundamental piece of biology that we were unaware of,” said Inigo Martincorena, a geneticist at the Wellcome Sanger Institute in Cambridge, England.
These lurking mutations went unnoticed for so long because the tools for examining DNA were too crude. If scientists wanted to sequence the entire genome of tumor cells, they had to gather millions of cells and analyze all of the DNA. A mutation, to be detectable, had to be very common.
But as DNA sequencing grew more sophisticated, Dr. Martincorena and other researchers developed methods for detecting very rare mutations, and they began to wonder if those mutations might be found in healthy cells, hidden below the radar.
Dr. Martincorena and his colleagues began their search in skin; its cells are battered daily by the sun’s ultraviolet rays, which trigger mutations. “We thought it was the lowest-hanging fruit,” Dr. Martincorena said.
In a study in 2015, he and his colleagues collected bits of skin left over from cosmetic surgeries to lift drooping eyelids. They examined 234 biopsies from four patients, each sample of skin about the size of a pinhead. They gently coaxed the top layers of cells, known as epithelial cells, from the underlying tissue.
Dr. Martincorena’s team then fished the DNA from the healthy epithelial cells, and carefully sequenced 74 genes that are known to play an important role in the development of cancer. Mutations that are common in cancer genes were remarkably common in these healthy skin cells, too, the researchers found. About one of every four epithelial cells carried a mutation on a cancer-linked gene, speeding up the cell’s growth.
It was possible, the scientists knew, that skin was peculiar. Maybe inside the body, away from the onslaught of ultraviolet rays, were healthy cells that didn’t carry these key mutations.
To find out, the researchers decided to study cells of the esophagus. The team gathered tissue samples from nine healthy organ donors who had died, then they sliced the tissue into dozens of tiny squares and examined the same 74 cancer-related genes.
Dr. Martincorena and his colleagues found that new mutations arose more slowly in the esophagus than in skin. But once those mutations emerged, they caused the esophageal cells to multiply faster than normal esophageal cells. Over time, these rogue cells spread out across the esophagus, forming colonies of mutant cells, known as clones. Although these clones aren’t cancer, they do exhibit one of cancer’s hallmarks: rapid growth.
“These mutant clones colonize more than half of your esophagus by middle age,” said Dr. Martincorena. “It was eye-opening for me.” Dr. Martincorena and his colleagues reported their findings on Thursday in the journal Science.
By examining the mutations, the researchers were able to rule out external causes for them, like tobacco smoke or alcohol. Instead, the mutations seem to have arisen through ordinary aging. As the cells divided over and over again, their DNA sometimes was damaged. In other words, the rise of these mutations may just be an intrinsic part of getting older.
“It seems that no matter how well one takes care of oneself by eating well, getting exercise and limiting certain vices, there’s likely only so much one can do against the need of the body to replace its cells,” said Scott Kennedy, a cancer biologist at the University of Washington who was not involved in the study.
The study also raised questions about efforts to detect cancer at its earliest stages, when cancer cells are still rare, Dr. Kennedy said: “Just because someone has mutations associated with cancer doesn’t mean actually they have a malignancy.”
Given the abundance of cancer mutations in healthy people, why isn’t cancer more common? Dr. Martincorena speculated that a healthy body may be like an ecosystem: Perhaps clones with different mutations arise in it, compete for available space and resources, and keep each other in check.
If so, fighting cancer might one day be a matter of helping harmless clones outcompete the ones that can lead to deadly tumors.
“There is no therapy being thought out in these terms now,” said Dr. Martincorena. “But I think it opens up new avenues. I think knowledge is always a weapon.”
Written by: Carl Zimmer
This article originally appeared on nytimes.com
Photo:Steve Gschmeissner/Science Source
A new study of women with ovarian cancer shows that ignorance about the condition is common among patients in all 44 countries surveyed. And that ignorance has a cost. The disease is more treatable, even potentially curable, in its early stages.
The women’s answers also suggested their doctors were ignorant. Many of them reported that diagnosis took a long time and that they weren’t referred to proper specialists.
The study was based on an online survey of 1,531 women who had been diagnosed with the cancer and was conducted by the World Ovarian Cancer Coalition, a nonprofit support group between March and May of this year.
Ovarian cancer is the eighth leading cause of cancer in women, according to the World Health Organization. Nearly 300,000 women will develop it this year. The World Ovarian Cancer Coalition estimates that one in six will die within three months of diagnosis and fewer than half will be alive in five years.
Prior to their diagnosis, two-thirds of the women surveyed either had never heard of ovarian cancer or were familiar with the name but didn’t know anything about the disease.
Amanda Tabral Vieira Benites, who now lives in São Paulo, is one of them. Six years ago, at age 21, she had no symptoms when she went in for a routine physical in the small city where she was living. Her doctor regularly did pelvic ultrasounds, not a common practice in the U.S. And he found something.
Eighty-six percent of Brazilian respondents knew little to nothing about ovarian cancer. Same with Benites. “At the time I knew exactly nothing about my cancer, nothing,” she says – despite her college education. She moved to São Paolo for access to better care. She’s got health insurance, and for her at least, “things went super-duper fast.” She went through four surgeries and six months of chemotherapy. She’s guardedly optimistic – the cancer has been gone for nearly five years.
Benites’ lack of noticeable symptoms was not unusual. When there are symptoms, they generally show up long after the cancer has started growing, and they’re nebulous – problems like abdominal bloating, indigestion, nausea, diffuse pain and low energy. In the survey, fewer than half of the women with ovarian cancer sought care within a month of when the symptoms first appeared. One in ten waited six months. Family history is a risk factor, yet only one in five women with a strong family history had had genetic testing.
In the survey, women from high-, middle- and low income countries who’d been diagnosed with ovarian cancer were asked by patient support organizations, their doctors or through social media to take an hour to fill out an online questionnaire about their experiences. Fifty seven percent were in stage 3 or 4 when diagnosed. Frances Reid, a study designer with the World Ovarian Cancer Coalition, says women in the survey were younger and likely to be more educated than the average woman with ovarian cancer, making the results likely to be a best-case scenario.
The survey also found that only about a third of the respondents had discussed clinical trials with their doctors.
The overall average time from first symptoms to diagnosis was 31 weeks — a couple of weeks shorter for the richer countries, a little longer for the poorer countries. But Hungary did better than the U.S. — 25 weeks as compared to 36 weeks. Among the high- and middle-income countries with enough data for statistical significance, Italy did best, with 62 percent of women diagnosed within a month of a first visit. The average was 43 percent. The U.K. was far behind at 30 percent. Germany was quick with diagnosis, but poor about access to specialists; the U.K. was the reverse.
“No one country does it well,” says Reid. “Different countries do different things well, but then they do other things not so well.”
“What they report is consistent with what we know about ovarian cancer,” says American Cancer Society epidemiologist Lindsey Torre, who recently wrote an overview of ovarian cancer in the US. “There’s not enough information out there.”
Some of the patients of Manas Chakrabarti, an Indian gynecological oncologist in Kolkata, participated in the survey. Chakrabarti says when he went to medical school many years ago, he was taught that ovarian cancer has no symptoms. Now he knows that it does but says many doctors around the world don’t. “Its symptoms are so subtle that unless your mind is open, your eyes don’t see,” he says.
The interviewees had, eventually, come in for care, where in many parts of the world people with cancer have no place to go. “If we can actually get data from people who did not get treatment or could not use a computer, the results will be absolutely devastating, I can assure you of that,” he says. “It’s much worse than it seems.”
“We need a lot more studies going on, on larger platforms,” Chakrabarti says. “We have a long road to travel.”
Joanne Silberner, a former health policy correspondent for NPR, is a freelance journalist living in London.
Written by: Joanne Silberner
Photo:iStock by Getty Images
This article was originally posted on NPR.com
 Recent news from the American Cancer Society (ACS), stating that women should start getting mammograms at age 45 instead of 40 has resulted in some confusion and uncertainty about clinical breast exams and mammograms. Maiya Hayes, who doesn’t have any family history of breast cancer was diagnosed in 2008 with stage 3 breast cancer at age 30. Hayes is living proof that ACS truly missed the mark with their “New Guidelines.”
Recent news from the American Cancer Society (ACS), stating that women should start getting mammograms at age 45 instead of 40 has resulted in some confusion and uncertainty about clinical breast exams and mammograms. Maiya Hayes, who doesn’t have any family history of breast cancer was diagnosed in 2008 with stage 3 breast cancer at age 30. Hayes is living proof that ACS truly missed the mark with their “New Guidelines.”
How was the cancer initially detected? (i.e. through a BSE, a CBE or an annual mammogram)
I discovered the malignant tumor in my right breast while doing a self-exam in November 2008. I’ve been doing self-exams for years because I had a benign breast tumor in that same breast when I was a teenager.
How much did you know about breast cancer (cancer period) before your diagnosis?
I knew very little about breast cancer and cancer period. I knew that breast cancer patients typically had a mastectomy and lost their hair and felt sick during chemo treatments. But that’s pretty much all I knew. I had no idea of how life-altering my cancer diagnosis would be.
How did you feel when you first received the news?
Honestly, I didn’t really understand how serious my situation was. So I didn’t cry or have an intense emotional reaction. I knew cancer had the potential to kill me, but because I was only 30, I didn’t think that would happen. I was naive, to realize how close to death I had come.
I knew I would need to have surgery, endure chemo and radiation treatments, and take some time off from work. But I didn’t realize I would end up being on medical leave for almost seven months.
Did you face any challenges during your treatment process? If so, how did you overcome them?
At first, my HMO insurance wouldn’t cover the anti-nausea meds that kept me from getting ill during my chemo treatments. The HMO wanted me to use a cheaper drug that didn’t help me at all. So for the first two months of my chemo treatments, my mom had to get my prescriptions filled via a mail-order pharmacy in Canada. Because Canada sells the drugs at a much cheaper rate than American pharmacies. And eventually after my mom wrote a letter to the HMO company, they finally agreed to pay for my anti-nausea meds.
Also, my paid medical leave expired at my job just as I was about to begin my radiation treatments. Since I needed to have an income to pay my bills, I returned to work full-time while undergoing my radiation treatments for eight weeks.
How has breast cancer changed your life?
My life is completely different in all aspects…
Emotional/spiritual changes
- I’ve always prided myself on being independent and not relying on other people for help. But getting cancer forced me to accept that everyone needs support, including me. And it made me realize that I wasn’t a weak person for asking for help.
- Anytime I have an ache or pain, or I feel more tired than usual, I worry that I’m sick again.
- I think about death and dying way more than someone my age should.
- I have a better relationship with God, and my spirit is stronger.
Physical changes
- I have to take Tamoxifen every day for 10 years to prevent the cancer from coming back. And because of those meds, the chemo and radiation, I have a lot of the symptoms of menopause – including hot flashes and issues with my short-term memory and remembering words.
- I have surgical scars from my chemo port, lumpectomy and lymph-node dissection. I have no feeling in my right armpit because of the lymph-node surgery. (So shaving is always an adventure. LOL)
- I always have to be very careful with my right arm because I’m at risk for lymphodema. So I can’t have any blood pressure tests or blood draws on my right arm.
- I’m usually cold, so cardigans and blankets have become my best friends.
- The texture of my hair completely changed when it grew back. So, now it’s super curly and very easy to wear naturally. My hair basically showed me that even in bad situations, something always positive happens.
Lifestyle changes
- I have to get mammograms, breast MRIs, pelvic ultrasounds and blood work every year to make sure I’m still cancer-free. I also have to see my oncologist every six months for check-ups.
- I notice every billboard, TV or radio commercial, or random sign or T-shirt that has the word “cancer.”
- My wardrobe has a lot more pink than it used to.
- I’m a member of Gilda’s Club Metro Detroit, an organization that helps cancer survivors with support groups, social gatherings and other uplifting events. Through Gilda’s, I’ve connected with other young survivors and made a whole new set of friends. A lot of the other young survivors are still battling cancer, so their experiences help me keep my self-pity or sad moments in check. And the past few years, several of my Gilda’s friends have died, so I’ve experienced lots of survivor’s guilt and sadness. But I hope I’m honoring their memories by not taking my remission for granted and making the most out of my life as I can.
What would you tell your younger self about cancer?
I would tell her that anyone can get cancer at any time. I would also tell her that cancer affects your mind and emotions just as much as it affects your body. So even when you go into remission, you’re never the same person you were before your diagnosis.
What message would you like to provide women/men in the community?
I would tell people in the community that no one is immune from getting cancer. Despite all the articles that say you can prevent it by eating healthier or exercising or”doing this” or “doing that,” there’s no absolute way to avoid getting cancer. It’s a complicated disease caused by many factors that are out of our control — like genetics and the environment. And statistics are meaningless because there’s a lot that the medical community doesn’t know about the disease. So it’s important to get your annual checkups and be aware of any changes in your health. Because all you can do is be vigilant.
The American Cancer Society just released an article/statement recommending the age for people to get a mammogram at the age of 45, if no family hx of breast cancer. What’s your take on this?
The new guidelines made me furious. I took it as a personal attack against me and the young friends I’ve lost to breast cancer. My friends and I are proof that people under age 45 who have no risk factors for breast cancer get it. I worry these guidelines will convince health insurance companies to stop covering yearly mammograms. And that would force many women to choose between paying $300 for a test that may or may not detect cancer, or saving that money to cover other life expenses.
If my ob-gyn hadn’t performed those exams on me, then I wouldn’t have learned how to do self-exams. And if I hadn’t done a self-exam back in November 2008, then I would’ve had terminal breast cancer by the time it was detected.

This year, Maiya participated as an art-bra model in Bras For A Cause, an annual fundraising event for Gilda’s Club Metro Detroit. The event involves breast cancer survivors modeling art bras, and it raised more than $100,000 for Gilda’s. She also served on the committee that helped organize the event.
Did you know that somewhere in the world, a woman is diagnosed every 19 seconds with breast cancer? Frightening isn’t it?! It is associated with obesity (LORD HELP ME!!), high-fat diet, sedentary life style, alcohol consumption, and can be increased if you have a genetic mutation (BRCA, which by the way, is more common in Black women and can be detected with a blood test-speak to your provider). There are clearly environmental contributors to the above-stated risks although these are hard to estimate. Meet several women who battled or is battling this disease and are determined to remain survivors.
Carrie Jordan
In 2016, Carrie was diagnosed with triple negative ductal carcinoma which is an aggressive form of breast cancer. She was given several rounds of chemo that really took a toll on her body, mind and soul followed by a double mastectomy and now back to chemo. Ye’s it’s been a journey, but she’s determined to keep fighting and for that mom, WE love and WE honor you!
Trina Stinson
Diagnosed with breast cancer in 2015, she’s definitely a survivor and WE honor her!
Michele Hammond
In 2012, Michele was diagnosed with metastatic breast cancer. As there’s currently no cure for her stage of disease, she remains optimistic and continues to liver her life. And for this, WE love and WE honor you!
Stacy Black
Stacy was diagnosed nine years ago with breast cancer. Now that she’s cancer FREE, she’s all smiles and going strong!
Maiya Hayes
At the age of 30, Maiya Hayes was diagnosed with stage 3 breast cancer after doing her own self breast exam. She’s been doing self-exams for years as she had a benign breast tumor in the same breast when she was a teenager. Age is truly nothing, but a number. Now that Maiya is cancer free, she’s definitely putting in the world by getting down in her Zumba classes!
Thank you ladies for sharing your stories as you all are warriors and survivors!