Heading Title
High levels of the carcinogen benzene were detected in a Houston neighborhood close to a Valero Energy refinery, local health officials said, heightening concerns over potentially hazardous leaks from oil and gas industry sites damaged by Hurricane Harvey.
Preliminary air sampling in the Manchester district of Houston showed concentrations of up to 324 parts per billion of benzene, said Loren Raun, chief environmental science officer for the Houston Health Department. That is above the level at which federal safety officials recommend special breathing equipment for workers.
Health officials also detected high levels of volatile organic compounds, which have been linked to a variety of health problems, including liver damage and cancer.
Dr. Raun said that monitoring would continue, and that some readings showed far lower levels of the pollutants, depending on which way the wind was blowing. Still, “these are high numbers,” she said.
The Environmental Protection Agency said it was also focusing on “an area of potential concern” linked to emissions from a Valero facility. E.P.A. air monitoring buses would continue to test pollution levels around the Valero refinery and others in the area as they start back up, David Gray, an agency spokesman, said in a statement.
Manchester, a low-income neighborhood hemmed in by two freeways, a shipping lane and the Valero refinery, has long suffered from industrial pollution. Researchers have found elevated levels of childhood leukemia in several areas in Houston, including Manchester, a plight blamed on high levels of chemicals in the air.
Valero Energy, a refiner based in San Antonio, had told local regulators that a floating roof covering a tank at its Houston refinery sank on Aug. 27 in the heavy rains brought by Harvey, causing benzene to leak into the air. The leak lasted only until the next day, Valero had said in its filing with the Texas Commission on Environmental Quality.
Since Aug. 23, 31 facilities in 10 counties have reported an estimated 4.5 million pounds of excess emissions to the commission, an analysis by the Environmental Defense Fund and Environment Texas shows.
Lillian Riojas, a Valero spokeswoman, said that a “hurricane ride-out crew” of Valero workers had made sure that the oil that escaped from the roof was “quickly contained” and that “cleanup is well underway.” Valero was coordinating with both federal and local environmental regulators to monitor any emissions from the oil, she said.
Benzene, a toxic, flammable chemical found in crude oil and gasoline, is known to cause central nervous system damage and bone marrow damage, and is carcinogenic.
Elena Craft, a senior health scientist at the Environmental Defense Fund, said continued monitoring was essential; there were “a lot of unknowns” related to how long communities might have been exposed to the pollutants, and at what sustained concentrations.
The health risks were clear, she said.
“For the short term, the risks are dizziness, nausea, lightheadedness. But this could also play into your long-term cancer risks,” she said. “We’re very concerned about people’s long-term health in the area.”
Article originally appeared on nytimes.com by: Hiroko Tabuchi
Image:Adrees Latif/REUTERS
Donald Jones used to pay at least $500 a month for a brand-name drug, Gleevec, that’s kept his leukemia at bay for five years.
Lately, he’s been paying almost as much for a generic version of the same pill.
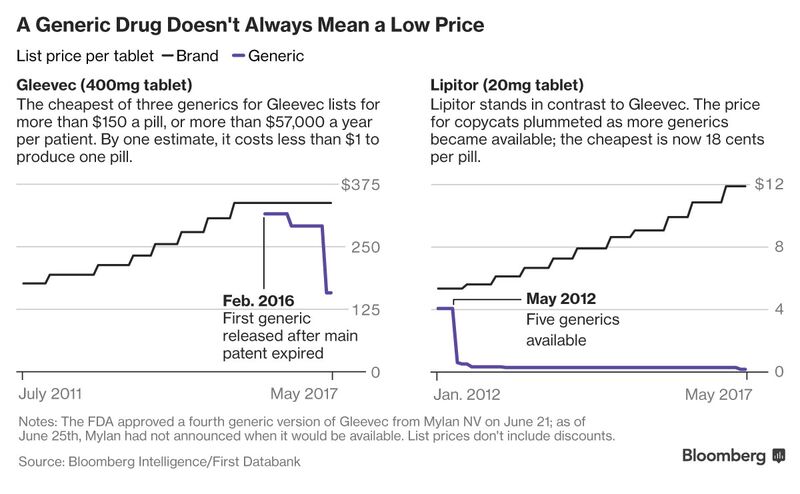
It’s not supposed to work that way. For decades in the U.S., generic drugs have been cheap, effective alternatives to expensive brand-name treatments. That’s changing with drugs like Gleevec, Novartis AG’s household-name cancer treatment. Generic forms of the drug can list for $150 or more a pill, before insurance covers part of that cost.
“If I don’t take it, I’m going to die,” Jones, 73, said in a phone interview. He lives in Desloge, Missouri and wants to retire from his $14-an-hour part time job refurbishing electric motors, which keeps him on his feet for hours. But he says he can’t, because he needs the money to pay for the generic version of a drug he thought would be far less expensive.
A handful of factors might explain the trend. Several large companies dominate the market for generics, potentially reducing competition. The starting prices of newer cancer drugs are higher than many mass-market treatments. And generics manufacturers said that pills for cancer can be more expensive to produce.
Jones’s frustration helps explain why U.S. consumers have made drug prices a major political issue. Democrats in Congress this month pushed President Donald Trump to hold to a promise to go after drug costs, and the Food and Drug Administration has also promised to take action to try and get prices of generics down.
“It is a very clear market failure,” says Andrew Hill, a researcher at the University of Liverpool who says that generic drugs should reflect their often inexpensive production costs. He calculates that a year’s worth of the cancer pills can be produced for under $350.
About 300 generic drugs had “extraordinary” price increases of 100 percent or more from 2010 to 2015, even as generic drug prices fell overall, according to a Government Accountability Office study of prices in Medicare. The report didn’t specifically focus on drugs like generic versions of Gleevec, which start at high prices and only come down gradually.
New Dynamic
“When a drug becomes generic, it should be treated like a commodity,” Hill said. For many drugs, that’s what happens. A 30-day supply of the generic version of Lipitor, Pfizer Inc.’s blockbuster cholesterol pill, lists for less than $20, compared to more than $350 for the brand.
Gleevec, approved in 2001, was considered a medical breakthrough that markedly increased the survival rate for patients with chronic myeloid leukemia. For a decade and a half, Novartis enjoyed exclusive sales rights, eventually charging about $10,000 a month before discounts. That made it a mega-blockbuster with $2.5 billion in U.S. sales in 2015. The list price for the cheapest generic version of Gleevec is still more than $4,700 a month, according to data compiled by First Databank and Bloomberg Intelligence.
Now that generic versions are available, Jones is using one that he hoped would lower his out-of-pocket costs dramatically. But after spending about $5,000 to get through the main part of his Medicare insurance plan’s drug coverage gap, he’s still spending $383 a month on a generic version made by Apotex Inc.
In the U.S., Sun Pharmaceutical Industries Ltd. is the leading provider of generic versions of Gleevec — making up about 42 percent of retail prescriptions for the once-a-day tablet, according to list price data from Symphony Health Solutions compiled by Bloomberg Intelligence. It charges $158 for each 400-milligram pill, according to data compiled by Bloomberg Intelligence, lower than other generic makers.
Sun said the cost of its generic is well below brand-name Gleevec and “has witnessed heavy erosion in its price.” Both Sun and Apotex say they have programs to help patients with commercial insurance afford out-of-pocket costs. Jordan Berman, an Apotex spokesman, said it’s “not accurate” to compare price dynamics for mass-market generic drugs to specialty medicines like Gleevec.
Few Competitors
The typical brand drug only has two generic competitors, fewer than in the early 2000s, according to an analysis by Rena Conti, an associate professor of health policy and economics at the University of Chicago, that was done with MIT researchers. At least three companies sell generic versions of Gleevec, including Teva Pharmaceutical Industries Ltd., along with Sun and Apotex.
Teva’s generic version of Gleevec lists for about $292, though the company said the actual amount it gets after discounts is far lower. Novartis says it has additional patents on its drug, including one on a form of the drug that expires in 2019. The company expects sales of brand-name Gleevec to continue to decline.
The FDA, which has in the past kept questions of drug costs at arm’s length, is starting to pay more attention. On June 5, FDA Commissioner Scott Gottlieb said the agency would take steps to get more competing generic drugs on the market, pushing applications to the front of the line when there are no, or only a few competitors.
Numerous other generics companies have filed applications to make generic versions of Gleevec, according to court filings against the companies by Novartis. The status of the other applications and why they haven’t moved forward isn’t clear, and the FDA declined to comment on the applications.
More Drugs
Gleevec isn’t the only cancer pill whose price has come down slowly despite losing patent protection. Prices for Targretin soared five-fold to $249 a capsule within two years of Valeant Pharmaceuticals International Inc. acquiring the rights in 2013. Mylan NV, one of the biggest generic drug manufacturers in the world, sells the only independent generic version of Targretin at a list price of about $215 per capsule, 14 percent less than Valeant’s.
Valeant, which sells its own generic version, says it’s not preventing other generic entrants.
Nina Devlin, a spokeswoman for Mylan, disagreed with Hill’s assessment that generic versions of cancer drugs are like other treatments. The pills are costlier to manufacture and require dedicated equipment, she said. Devlin said Mylan sells 635 drugs in the U.S. at an average price of 25 cents a dose.
A typical two-week cycle of Roche Holding AG’s Xeloda, a colon cancer drug, cost more than $3,000 when it lost patent protection in 2014. Today, six generic companies make versions of the drug. Their list prices range from $560 to $2,628 for the same two-week cycle of drugs.
Cindy Coor, 45, of Mount Olive, North Carolina, was prescribed Xeloda after being diagnosed with a rare form of cancer in the lining of her abdomen this spring. She said she couldn’t afford the $200 co-pay and takes an alternative drug, infused through a catheter in her chest.
“What is the point of it being generic if you are going to have to pay $200?” she said.
This article originally appeared on bloomberg.com by Robert Langreth and Daniel Levitt
Photo: iStock
As our writer Deanna has described, nothing can really prepare you for the side effects that come with cancer treatment. It’s common knowledge that hair loss can happen, but it’s another thing to wake up one day and realize you have no more eyebrows. (Really, you should read her account of it—it’s both eye-opening and endearing.) That’s why Sephora’s latest addition to its Classes for Confidence series, called Brave Beauty in the Face of Cancer, is great news for women and men undergoing chemo who want to talk to others who get it—and pick up some tips on how to pencil in their brows along the way.
The series, if you’re not familiar, centers around creating free classes for people going through major life transitions (like, say, fighting cancer). The classes kicked off on Sunday, April 9, in select stores and feature a curriculum shaped by input from Sephora employees who are also living with cancer. The goal, according to Corrie Conrad, senior director of social impact and sustainability for Sephora, is “to create a safe place for participants to learn and play with beauty, ask questions, and connect with others going through a similar situation.” On the “syllabus” for the 90-minute class: skin care tips, step-by-step instructions for upping radiance, creating natural-looking brows, and tricks for defining your eyes.
Safe to say, it seems like it’s already a hit with both the instructors and the students, as evidenced by a video the company released featuring moments from a preview class. Sephora employee Emily starts the clip with “When I heard that these classes could be a possibility with Sephora, it hit me maybe this is why I’m here and this is the reason why I survived.” And participant Amy says, “By having some confidence with things I can do with makeup, it’ll help me get out and be with people I need to be with.”
Check it out in full below.
The initiative extends outside of the classroom too. As a show of solidarity, Sephora employees who are going through or have completed a cancer journey are given the option of wearing a lapel pin featuring a heart logo to both foster a sense of community and give customers an opening if they have questions about their own cancer-treatment-related beauty concerns.
You can get more info on class locations and sign ups here. Beauty really is so much more than playing with lipstick or eyeshadow palettes. It’s great to see brands using their platforms to get at the heart of how makeup can be deeply transformative.
This article originally appeared on glamour.com, Beth Shapouri
Photo: Mark Metcalfe
After learning he had early stage prostate cancer, Paul Kolnik knew he wanted that cancer destroyed immediately and with as little disruption as possible to his busy life as the New York City Ballet’s photographer.
So Mr. Kolnik, 65, chose a type of radiation treatment that is raising some eyebrows in the prostate cancer field. It is more intense than standard radiation and takes much less time — five sessions over two weeks instead of 40 sessions over about two months or 28 sessions over five to six weeks.
The newer therapy is surging in popularity, but no one knows whether it is as effective in curing prostate cancer, or how its side effects compare.
The rise of short-course radiation is an example of the evidentiary blind spots that bedevil the treatment of prostate cancer. It is second only to lung cancer in men, striking 180,000 patients a year. But treatments for lung cancer, and for other common cancers like those of the breast and colon, have been evaluated in randomized clinical trials more often than those for prostate cancer.
The number of men getting the short, intense treatment, called stereotactic body radiation therapy, or S.B.R.T., more than doubled to 1,886 in 2013 from 716 in 2007, according to the most recent Medicare data. The number of men getting standard radiation therapy fell over that same time period, according to Medicare, to 47,512 from 66,549.
The National Cancer Institute has just agreed to fund a clinical trial that researchers hope will settle which treatment is better. It will randomly assign 538 men to have either a short course of five intense radiation sessions over two weeks or 28 treatments over five and a half weeks, comparing outcomes for quality of life as well as disease-free survival.
But it will be at least eight years before the answers are in. In the meantime, men and their doctors are left with uncertainty.
“Ideally, we want to show five treatments is better,” said Dr. Rodney J. Ellis, a radiation oncologist at Case Comprehensive Cancer Center in Cleveland and the principal investigator for the trial.
One reason for the dearth of data is that prostate cancer usually grows slowly, if at all, so it can take many years to see if a treatment saved lives. It is expensive and difficult to follow patients for such a long time, and the treatments given to the men often change over a decade, making doctors wonder if the results are relevant.
Also, researchers who have tried to conduct studies comparing treatments often failed because specialists were already convinced that the method they used was best and were reluctant to assign men to other treatments. Dr. Ian Thompson of the University of Texas Health Science Center in San Antonio, said he was involved with several clinical trials that withered for that reason.
For men, quality of life is often pivotal in choosing a treatment, weighing which possible side effects sound worse: with surgery, urinary incontinence and impotence; or, with radiation, bowel problems including diarrhea and rectal leakage, and impotence. With the shorter radiation treatment, there is also a possibility that scarring can block the urethra, an effect that might not emerge until years after the treatment.
In the absence of a broad base of solid evidence, men often make decisions based on personal preferences or on the advice of a trusted doctor. Like Mr. Kolnik, some want as short a recuperation as possible and find the newer kind of radiation treatment appealing.
But prostate cancer specialists worry about the lack of data.
Dr. James Yu, a radiation oncologist at Yale, who will lead the quality of life assessment for the new clinical trial, says crucial unanswered questions are, “How fast can you give it and how fast is too fast?”
Very high dose radiation was studied in the treatment of lung cancer, said Dr. Anthony V. D’Amico, a radiation oncologist at Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston. For lung cancer patients with small tumors that are not near sensitive structures, like large blood vessels, it appears to be just as curative as surgery.
But lung cancer is easier to treat because, with properly selected patients, doctors can avoid sensitive tissues — all the oncologist has to worry about is hitting the cancer.
Not so with prostate cancer.
“The urethra is within the prostate and the bladder neck is literally touching to top of the prostate,” Dr. D’Amico said. Also, the rectum is directly behind the prostate. Radiation can damage those other tissues, he said.
Injuries to the urethra and bladder neck might not show up until five or 10 years after the treatment, Dr. D’Amico noted. Those structures can scar and close, limiting the flow of urine. It also can take years before rectal scarring produces symptoms like bleeding.
A few years ago, Dr. Yu and his colleagues looked at Medicare data and reported that men who had more intense radiation therapy were more likely to have urinary problems after two years than those who had the longer-course therapy.
Dr. Yu noted that his study was not a randomized trial, the gold standard, but he said the results were not reassuring. Now, though, he is not so sure the intense therapy is worse.
“In my own experience, these men have done really well,” he said. “That tells us that techniques improved, or the medical claims we evaluated were not indicative of major toxicity, or the way we and others at high-volume centers deliver radiotherapy is different.”
The lack of solid data bothers Dr. Daniel W. Lin, chief of urologic oncology at the University of Washington. When men ask him about the shorter radiation course, he tells them, “It probably can work but it doesn’t have long-term results and it hasn’t been tested against standard radiation.”
At centers like Sloan Kettering, doctors are relying on their own experience.
Dr. Michael J. Zelefsky, a radiation oncologist who treated Mr. Kolnik there, said that several years ago, 90 percent of his patients had the standard course of treatment. Now 90 percent choose the shorter course. On the basis of Sloan Kettering’s experience with several hundred men who had the intense radiation therapy over the past three years, the treatment, he said, “is emerging as a very exciting form of therapy.”
Mr. Kolnik is more than satisfied.
During his treatment, he said, “I totally kept up with my schedule.” He did not even tell anyone other than a few close friends that he was having radiation therapy.
“The treatment begins and it finishes before you even realize it,” Mr. Kolnik said.
Nine deaths have been reported to the US Food and Drug Administration stemming from a rare cancer that is associated with breast implants.
The extremely rare cancer, called anaplastic large cell lymphoma, affects cells in the immune system and can be found around the breast implant. It can be found in the skin or lymph nodes and is not a type of breast cancer.
“All of the information to date suggests that women with breast implants have a very low but increased risk of developing ALCL compared to women who do not have breast implants,” the FDA reported.
On Tuesday, the FDA issued an update on its understanding of breast implant-associated ALCL cases.
The agency has received 359 reports of possible breast implant-associated cancer cases as of February 1. But the exact number of cases “remains difficult to determine due to significant limitations in world-wide reporting and lack of global implant sales data,” it said.
What science shows in the past six years
In 2011, the FDA first raised the possibility of a small but significant risk of developing the cancer after getting breast implants. It asked doctors whether they noticed changes in their patients and for women to check for symptoms such as fluid buildup, hardening or a mass around their implants. Symptoms of the cancer also include swelling and redness around the breast implants.
Since that report six years ago, the scientific community has learned more about the link between breast implants and ALCL.
Most of the cancer cases occurred in people who had textured surfaces on their implants, rather than smooth surfaces. Of the 231 reports to the FDA that contained information about the implant, 203 had textured surfaces.
Most cases of ALCL have been described as a slow-growing and treatable when it’s detected early.
About 10 million to 11 million women in the world have breast implants, according to the American Society of Plastic Surgeons and the Plastic Surgeon Foundation. Fewer than 10 patients are diagnosed each year with breast implant-associated ALCL, and one study estimated an incidence of 1 in 300,000, according to the two groups.
What to do if you have breast implants
Breast implants remain incredibly popular. It’s the top cosmetic surgery performed in the US, with 290,467 procedures in 2016, according to the American Society of Plastic Surgeons.
People who are considering getting the surgery should do their research and discuss with their surgeons about the risks and benefits of textured- and smooth-surfaced implants, the FDA advised.
People who have breast implants should monitor their implants for any changes and get routine screenings such as mammograms or MRIs as recommended by their doctors, the agency suggested.
This article originally appeared on cnn.com by Madison Park
Photo: Wikimedia Commons
A new blood test can locate the presence of a tumor in a particular tissue, which may circumvent the need for invasive procedures such as biopsies and aid in cancer diagnosis according to a recent study published in Nature Genetics.1
Cancer blood tests detect cancer by screening for traces of DNA released by dying tumor cells. However, they do not provide information about the location of the tumor. “Knowing the tumor’s location is critical for effective early detection,”
said Kun Zhang, a bioengineering professor at the University of California San Diego Jacobs School of Engineering and an investigator on the recent study.
The investigators identified the location of a tumor using CpG methylation haplotype, a type of DNA signature. CpG methylation is the addition of methyl groups to CG sequences in DNA. Each tissue can be identified by its unique collection of methyl groups, known as a methylation haplotype. As a tumor grows it competes for nutrients and space in the tissue, causing normal cells to die. DNA from dying normal cells released into the bloodstream can then be used to identify tumor location using methylation haplotype.
“We made this discovery by accident. Initially, we were taking the conventional approach and just looking for cancer cell signals and trying to find out where they were coming from. But we were also seeing signals from other cells and realized that if we integrate both sets of signals together, we could actually determine the presence or absence of a tumor, and where the tumor is growing,” explained Zhang.
The researchers created 2 databases: one of tissue CpG methylation patterns (liver, intestine, colon, lung, brain, kidney, pancreas, spleen, stomach, and blood), and the other of cancer-specific genetic markers. The test requires both cancer-specific genetic markers and a tissue specific methylation pattern above a statistical cutoff to assign a positive match.
This article originally appeared on Oncologynurseadvisor.com
Photo:Torange.biz
Winship Cancer Institute medical oncologist Omer Kucuk, MD, has authored an editorial in the journal Cancer that recommends women consume soy foods to help prevent breast cancer and improve the prognosis of those currently undergoing treatment. Kucuk, who is an expert in integrative medicine, nutrition and cancer prevention, has studied the use and impact of soy isoflavones for more than two decades.
Kucuk says “we now have evidence that soy foods not only prevent breast cancer but also benefit women who have breast cancer. Therefore, we can recommend women to consume soy foods because of soy’s many health benefits.”
Soy isoflavones are known to have cancer-fighting properties that include epigenetic, metabolic, immunologic and anti-inflammatory effects. To get the maximum benefit of soy isoflavones, Kucuk explains that they should be regularly consumed throughout a person’s lifespan. As an integrative medicine expert, he also emphasizes that soy protein and isoflavones are among the best functional foods and nutraceuticals for preventing treatment side effects and improving quality of life of cancer patients and survivors.
This article originally appeared in the Journal Cancer by Omer Kucuk, MD
Photo:Wikimedia Commons
Tabay Atkins is a typical sixth-grade boy. He loves building Legos and counts math, social studies and English as his favorite subjects in school.
The 11-year-old from San Clemente, California, also happens to be an in-demand yoga instructor who teaches classes three days per week.
“I care about people and a lot of people really like taking my classes,” Tabay told ABC News. “I think I’m inspiring and a lot of people just like my story.”
“And I don’t judge people,” he added of his appeal as an instructor.
Tabay’s yoga journey began when he was just 6 years old. His mother, Sahel Anvarinejad, took a yoga teacher training program to help herself recover from non-Hodgkin lymphoma.
“By accident I got into yoga after I ended chemotherapy treatments,” Anvarinejad, 37, told ABC News. “Tabay was with me every step of the way.”
“He went to the trainings and he saw how it changed me,” she said. “I was lighter. I didn’t have the heaviness that cancer brings.”
When Tabay graduated from fifth grade last spring, Anvarinejad gave her son the choice between a trip to Europe or the chance to undergo a 200-hour yoga teacher training program himself.
“He chose training without hesitation,” Anvarinejad, now cancer free and the owner of her own yoga studio, said of her son. “He said, ‘Mom I want to do this too. I want to teach people so yoga can help them the way that yoga helped you.’”
Tabay began an intensive instructor program that consisted of nearly 12 hours of instruction every day from Los Angeles-based YOGAthletica trainer Shana Meyerson.
“Tabay was nothing short of extraordinary,” Meyerson told ABC News. “He took in all the information, and regularly exhibited a deep and fundamental understanding of the material.”
She added, “Even my toughest questions—that no one else could answer—were consistently and correctly answered by Tabay.”
Tabay was the youngest person ever to complete Meyerson’s 200-hour YOGAthletica Teacher Training, with the closest in age being 24, according to Meyerson.
“The adults in the training, all women, treated him with a unique combination of maternalism and peer respect,” she said. “Somehow he managed to immerse himself in this very grown up world and never lose his childlike innocence and sense of wonder, and fun.”
Tabay now teaches classes two days per week after school and on Saturdays at his mom’s studio. Often by his side in his yoga classes are his mom and dad, former NFL player Larry Atkins.
“Before he started yoga with me he wasn’t flexible because he didn’t do yoga when he played football,” Tabay said. “And after doing yoga with me a lot he’s becoming a lot more flexible and he’s a lot happier.”
Tabay’s classes are donation-only and he gives the proceeds to charities supporting children with cancer, the family said. Their studio, Care4Yoga, also waives the normal $30 per class drop-in fee for all cancer patients and their family members.
“People leave in tears because they’re that touched,” Anvarinejad said of her son’s classes. “There’s just a connection he has with everybody on every level, it’s just something else.”
Tabay has taught yoga classes around the world and also teaches his classmates at school.
“It’s really awesome,” he said. “Some of the boys at first when I tell them that they should try yoga, they say no because they think it’s for girls but yoga was actually created by men, for men.”
As he gets older, Tabay plans to keep expanding his yoga outreach.
“I want to try to open up as many studios as I can and spread the yoga word,” he said. “Yoga helps in a lot of ways…I want to teach yoga to anyone and everyone I can.”
This article originally appeared on abcnews.com by: Katie Kindelan
Photos:Sahel Anvarinejad
Sharon Jones, an iconic Grammy-nominated soul and funk singer who rose to fame relatively late in life, died on Friday of pancreatic cancer. She was 60.
Jones, known for her high-spirited live shows, passed away at a hospital in upstate Cooperstown, surrounded by her bandmates, according to a representative.
“We are deeply saddened to announce that Sharon Jones has passed away after a heroic battle against pancreatic cancer,” a statement on the singer’s website said. “She was surrounded by her loved ones, including the Dap-Kings.”
Born in Augusta, S.C., Jones was raised in Bedford-Stuyvesant, Brooklyn.
Jones struggled to earn money as a gospel singer and session vocalist in her 20s and 30s, and worked for years as a correction officer at Rikers Island and drove armored cars for Wells Fargo Bank.
The enigmatic vocalist released her first album at 40 after providing backup vocals for soul legend Lee Fields.
Jones befriended Gabriel Roth, one of the organizers of the Fields sessions.
Roth later started Daptones Records and made Jones one of his top stars.
She earned critical acclaim as the fiery frontwoman of the group Sharon Jones & the Dap-Kings, blowing away audiences with her sweet, soulful vocals and her tireless stage presence.

ones was the subject of a documentary released this summer, “Miss Sharon Jones!” (MATTHEW EISMAN/GETTY IMAGES)
The band released seven albums together smothered in guitar licks and horn blasts straight out of the ’60s and ’70s.
She was nominated for her first Grammy in 2014 for best R&B album for “Give the People What They Want.”
Jones lived with her mother, Ella Mae Price Jones, in Far Rockaway for years, even after she became a sensation in the soul revival scene.
“The fabulous Sharon Jones has passed tonight she & her band The DapKings made great music together & she sang her butt off. Condolences RIP,” Whoopi Goldberg tweeted Friday.
“#RIPSharonJones – You are incredible and mighty. Condolences to your family,” guitarist Nile Rodgers wrote.
The Roots drummer Questlove shared a photo of a defiant-looking Jones and simply wrote, “Thank You Sharon. Thank You. #2016.”
The sultry singer was diagnosed with pancreatic cancer in 2013, but went into remission and continued to tour and record music. The cancer returned in 2015 and spread to other parts of her body.
Jones was the subject of a documentary released this summer, “Miss Sharon Jones!,” that chronicled her battle and initial recovery from cancer.
This article originally appeared on New York Daily News.com; by: Denis Slattery
Ifill, 61, broke gender and racial barriers and became a role model for journalists across the country. She had been battling endometrial cancer while covering this year’s presidential election.
PBS said in a statement that she died Monday “surrounded by family and friends.”
“Gwen was one of America’s leading lights in journalism and a fundamental reason public media is considered a trusted window on the world by audiences across the nation,” Paula Kerger, the PBS president and CEO, said.
“She often said that her job was to bring light rather than heat to issues of importance to our society,” Kerger said.
Ifill, who worked at The Washington Post, The New York Times and NBC News, became moderator of PBS’s “Washington Week in Review” in 1999. She was tapped to be the co-anchor of the “NewsHour” in 2013. Ifill and co-anchor Judy Woodruff were the first women to jointly lead a national nightly news broadcast.
Ifill also moderated the 2004 and 2008 vice-presidential debates, as well as a 2016 Democratic primary debate.
“I think we’re all diminished without Gwen,” CNN’s Gloria Borger, a longtime friend of Ifill’s, said after the news of Ifill’s passing was announced.
Borger recalled that Ifill’s “preparation for those debates was stunning.”
“She was such a role model for me, and for so many people,” CNN’s Nia-Malika Henderson said.
“We all loved her,” CNN’s Jamie Gangel said, remembering Ifill as smart, funny and fearless.
Ifill was a pioneer for women and for African Americans in journalism, becoming the first African American woman to host a major political talk show when she took the helm at “Washington Week in Review.”
Her path to prominence was hard-fought: While in college in the late 1970s, Ifill secured an internship at The Boston Herald.
“They didn’t know what a college-educated black woman was and they didn’t know how to treat me,” she once told The Washington Post. One day, she told the Post, a staffer left her a note in the photo lab that said “Nigger go home.” The editors were so apologetic about the issue that they hired Ifill after her 1977 graduation, she recalled.
Ifill was scheduled to receive a prestigious award, the John Chancellor Award, at a Columbia University ceremony on Wednesday.
In a telephone interview, Ifill’s close friend Michele Norris remembered her as a dedicated journalist, someone who stayed true to the values of her craft amid wrenching changes across the news industry.
Ifill was diagnosed with cancer sometime at the end of 2015 or early in 2016, Norris said.
Ifill shared the news with family and friends but chose to keep the cancer battle private. In April, she had to take a leave of absence from the “NewsHour,” for what were described as “ongoing health issues.”
Norris said Monday that this absence was due to complications from the treatment.
She returned to work in May, and within weeks she had an exclusive interview with President Obama.
But Ifill was forced to take another leave of absence last week. She was at hospice care in Washington, D.C. when she died on Monday, according to Sharon Percy Rockefeller, the president and CEO of WETA, which owns the “NewsHour.”
“I spent an hour with her this morning and she was resting comfortably, surrounded by loving family and friends,” Rockefeller said in an internal memo.
Rockefeller said she “conveyed to Gwen the devoted love and affection of all of us at WETA/NewsHour. Let us hold Gwen and her family even closer now in our hearts and prayers. I have loved knowing and working with Gwen and will always cherish her memory.”
Article originally published: Dylan Byers and Brian Stelter (CNN Money Los Angeles)
Photo: Getty Images













