Heading Title
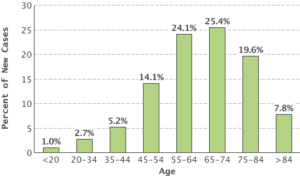
Advancing age is the most important risk factor for cancer overall, and for many individual cancer types. According to the most recent statistical data from NCI’s Surveillance, Epidemiology, and End Results program, the median age of a cancer diagnosis is 66 years. This means that half of cancer cases occur in people below this age and half in people above this age. One-quarter of new cancer cases are diagnosed in people aged 65 to 74.
A similar pattern is seen for many common cancer types. For example, the median age at diagnosis is 61 years for breast cancer, 68 years for colorectal cancer, 70 years for lung cancer, and 66 years for prostate cancer.
But the disease can occur at any age. For example, bone cancer is most frequently diagnosed among people under age 20, with more than one-fourth of cases occurring in this age group. And 10 percent of leukemias are diagnosed in children and adolescents under 20 years of age, whereas only 1 percent of cancer overall is diagnosed in that age group. Some types of cancer, such as neuroblastoma, are more common in children or adolescents than in adults.
Percent of New Cancers by Age Group: All Cancer Sites
Article originally posted on cancer.gov
The largest study ever to investigate how genetic and biological factors contribute to breast cancer risk among black women launched today. This collaborative research project will identify genetic factors that may underlie breast cancer disparities. The effort is funded by the National Cancer Institute (NCI), part of the National Institutes of Health.
The Breast Cancer Genetic Study in African-Ancestry Populations initiative does not involve new patient enrollment but builds on years of research cooperation among investigators who are part of the African-American Breast Cancer Consortium, the African-American Breast Cancer Epidemiology and Risk (AMBER) Consortium, and the NCI Cohort Consortium. These investigators, who come from many different institutions, will share biospecimens, data, and resources from 18 previous studies, resulting in a study population of 20,000 black women with breast cancer.
“This effort is about making sure that all Americans – no matter their background – reap the same benefits from the promising advances of precision medicine. The exciting new approaches to cancer prevention, diagnosis, and treatment ring hollow unless we can effectively narrow the gap of cancer disparities, and this new research initiative will help us do that,” said Douglas R. Lowy, M.D., acting director of NCI. “I’m hopeful about where this new research can take us, not only in addressing the unique breast cancer profiles of African-American women, but also in learning more about the origin of cancer disparities.”
Survival rates for women with breast cancer have been steadily improving over the past several decades. However, these improvements have not been shared equally; black women are more likely to die of their disease. Perhaps of most concern is that black women are more likely than white women to be diagnosed with aggressive subtypes of breast cancer. The rate of triple-negative breast cancer, an aggressive subtype, is twice as high in black women as compared to white women.
The exact reasons for these persistent disparities are unclear, although studies suggest that they are the result of a complex interplay of genetic, environmental, and societal factors, including access to health care. Large studies are needed to comprehensively examine these factors, and NCI is supporting several such efforts.
As part of the study, the genomes of 20,000 black women with breast cancer will be compared with those of 20,000 black women who do not have breast cancer. The genomes will also be compared to those of white women who have breast cancer. The project will investigate inherited genetic variations that are associated with breast cancer risk in black women compared to white women. In addition, researchers will examine gene expression in breast cancer tumor samples to investigate the genetic pathways that are involved in tumor development.
“This $12 million grant—in combination with previous investments—should help advance our understanding of the social and biological causes that lead to disparities in cancer among underserved populations,” said Robert Croyle, Ph.D., director of NCI’s Division of Cancer Control and Population Sciences (DCCPS), which is administering the grant. “A better understanding of the genetic contributions to differences in breast cancer diagnoses and outcomes among African-Americans may lead to better treatments and better approaches to cancer prevention.”
“A number of studies have suggested that genetic factors may influence breast cancer disparities, so we’re hopeful that this project can help to shed further light on this matter.” said Damali Martin, Ph.D., program director for the DCCPS Genomic Epidemiology Branch. Dr. Martin’s office is working directly with the grant recipients as well as the consortia groups that have been researching black women and breast cancer.
The grant has been awarded to Wei Zheng, M.D., Ph.D., of Vanderbilt University, Nashville, Tennesee; Christopher Haiman, Sc.D., of the University of Southern California, Los Angeles; and Julie Palmer, Sc.D., of Boston University. Additionally, minority scientists from various institutions, including from one Historically Black College and University medical school, are playing an important role in this study, and they have been involved in previous research that this study builds upon. For example, the Southern Community Cohort Study, a contributing study for this grant, represents a 15-year partnership between Vanderbilt and historically black Meharry Medical College in Nashville, Tennessee. In addition, this grant will provide training opportunities for scientists from minority populations.
Support for ongoing research in this area represents NCI’s continued commitment to fund a comprehensive portfolio of research aimed at reducing cancer risk, incidence, and mortality, as well as improving quality of life for cancer survivors across all demographic groups.
Article originally posted on cancer.gov
Photo Credit:IStock
All week leading up to the 6th Annual Winship Cancer Institute 5k race with Emory University, some friends and I participated in the Workweek Hustle Challenge via Fitbit. By the way, I won the challenge (80k plus steps).
I was extremely tired and wanted to quit, but I couldn’t because I usually keep my word. Friday came and it was time for me to help with registration. After hours of getting participants ready for the race it was time for me to head on home. My feet were tired and my legs were aching, it felt like I’d participated in several cross-fit and boot-camp classes. I finally made it home to rest and thought to myself “what have I got myself into, with this race?” Not only had I planned to participate in the 5k, I offered my services to the registration table prior to the race.
MORNING OF THE RACE…
The alarm goes off, its 5am. I’m lying in bed thinking, “I don’t want to go, I can’t get up, I’m soooo tired!” I honestly felt if my friend Holguine weren’t participating in the race with me, I would’ve thrown up the deuces and gone back to sleep.
Once we arrived on campus, I felt energized and excited to be apart of something meaningful. I was extremely happy to have followed through with this years 5K.
I’ve participated in plenty of cancer related and non-cancer events, but for some reason this one felt much different. At this point I couldn’t figure it out, so I kept working.
RACE TIME…
It was time for me to get in “FORMATION,” (all you Beyoncé’ fans aka the #BeyHive, I finally said it…LOL) for the race. The Grand Marshal fired the race shots & we were off. I started to run, yes I said RUN!!! It was a slow and steady pace, but I ran.
The first mile was something else I tell you. No Crystal C. Jordan did NOT run that entire mile, but she did have a constant jog which is more than she’s ever had in her adult life. I was proud of myself.
As mile two approached, I was tired and felt I couldn’t go on. I wanted to stop; actually I wanted to lie down for a little while. I kept thinking, “where’s the third mile marker, cause this “sista” isn’t going to make it!” Holguine and I kept going; of course we’re walking at this time. I wanted to complain, but I didn’t. Thinking about my father, uncles, aunt, friends, others who fought and or were fighting cancer, I had to keep going.
I thought to myself, how dare I complain about a three plus mile race “I” volunteered to be apart of when NO ONE decides to be diagnosed with cancer and to go through numerous surgical operations, chemo, radiation, losing their hair, finger nails, loss of feeling in their finger tips or dealing with excruciating pain that most couldn’t imagine all the while praying to their God in hopes of becoming cancer free.
As one of my favorite entertainers, Sean “Puff Daddy” Combs would say; “Can’t Stop, Wont Stop!” That’s what I did; I kept going. Sure my legs and feet were aching, but I knew I could do this.
There was so much support and encouragement out. From route monitors to all the people on the sidelines, & supporters cheering everyone along the way. I gained more energy and became a little emotional. Why you may ask? For the simple reason, we all have dealt with some type of pain, or disappointment, publicly or privately and to have someone, for that matter a stranger who doesn’t know your struggle giving you words of encouragement and support. My soul filled with so much joy and gratefulness.
Whoever said support from others isn’t necessary for one to succeed. In my opinion, they LIED!!! There’s no one in this world that gained success on his or her own. EVERY person needs to “hear “words of encouragement throughout their individual journeys. If you disagree with that statement, please bring a list of names and their solo accomplishments.
MILE THREE IS NEAR…
Finally I made it to mile three and could see the finish line near. I finished the 5k in less than an hour. Many of you may say, “it took you that long, or I wouldn’t share that time.” That’s YOU because I’m PROUD of the time I finished with. All because I was apart of something meaningful and that I ran/jogged more than I’ve ever done. So this was actually a milestone for ME.
During the race I felt empowered, loved and grateful. With so many unpleasant things’ happening on a daily, I was proud to see there wasn’t any division. Everyone who came out was supportive of one another. We were in a fight together, the battle against cancer. One that I pray will be over sooner than later.
Since releasing her debut album, Dap Dippin’ with Sharon Jones and the Dap-Kings, in 2002, soul singer Sharon Jones has become a driving force in her genre. Although Jones, now 60, gained prominence later in life than many musicians, she has spent the last decade and a half bringing her charismatic, horn-laden, funk-infused brand of soul to audiences throughout the world via a tireless touring schedule and seven studio albums.
But after years spent toiling to break into the music industry, Jones faced a different challenge in 2013. That year, the singer was diagnosed with pancreatic cancer and underwent extensive treatment. Jones overcame the illness and returned to the stage in 2015 — a comeback chronicled in the new Barbara Kopple documentary, Miss Sharon Jones!, which hit theaters late last month.
Jones, however, received tough news in May when doctors found cancer cells in her stomach, lymph nodes, and lungs. When EW connected with her by phone to discuss the documentary and its companion soundtrack — out Friday and featuring the new song “I’m Still Here” — Jones had just resumed radiation therapy. “I’m sitting here on the bed now,” she said. “I went to walk up the steps, and my legs felt like lead.”
Despite her diagnosis, Jones was optimistic — she sees herself as a fighter and emphasized that she has more music in the works than ever. Below, EW speaks with Jones about drawing inspiration from James Brown, finding strength in humor, and potentially releasing a gospel album.
How are you feeling these days?
I’m feeling alright. One of the reasons why I had to cancel the European [tour], [was] because of the radiation. I would’ve been leaving the next day, and I couldn’t deal with that. I don’t know what effects it’s going to have on me. I know the chemo makes me tired, and radiation is going to make me even tired-er. It hurt me to [cancel the shows], but I had to. But I’ll be alright. They’ll see me again soon. It’s all about the willpower.
How have people been reacting to the documentary?
Nothing but great reviews. It’s just been announced it’s going to be [screening] in Augusta, in my hometown, in September. To get to see it in Augusta — that’s like coming home.
The film has some moving details about your experience growing up there in segregation. What’s it like to know it’ll be showing there?
It’s hard to get people in your own hometown to accept you, believe it or not. James Brown, even with all the things he’d done, some people were a little slow about coming out [when he would perform in the South]. I was [in Augusta] and I couldn’t even sell out the Imperial Theatre. It’s a little heartbreaking, but he still loved his home and he still did what did. And the same with me: Whether they come out or not I still love my home. But to hear the hoopla and the build up about [the documentary]? Yeah, I’m excited. The thing I like about home, when they see you, they just speak to you. They see me and they speak and they keep going.
How did you decide to let Barbara Kopple and her team into your very personal health struggle?
Barbara, you look at her and who could tell her “no”? She has a passion for getting into it and getting stuff out of people. Once I accepted and said they could do it, you forget they’re there sometimes. I didn’t want it to be one of those reality shows. If they would’ve caught me in the morning — like, “Yawn! Sharon’s waking up!” — that’s a reality show, to me. You don’t need any of that. Whatever I asked them not to have on film, they did not have on film.
Barbara did a great, great job. We’re going to be friends forever. Even after we finish all this, we’re still going to be talking to each other.
In the documentary your sense of humor really comes through. How has that helped you throughout your career and this battle with cancer?
People always told me I’ve always been funny, even in school. Some people told me a long time ago, “You know, you should’ve been a comedian.” I’ve always been funny and I love doing that. Humor, laughter, it eases the pain.
What motivated you to keep trying, for so many years, to break into the music industry?
I said, “One day they will pick me for my voice, and not for the way that I look. They’ll see I can sing and it has nothing to do with the way I look.” I never got away from music. I had to always be a fighter. It’s always been like that. I’m a fighter, and I keep my faith and my belief.
What music do you have in the works?
We always have stuff coming up, because those guys [in the Dap-Kings] are always writing songs. We’re going to have a new album out soon — next year — so that when we’re touring we have new material. As we start finishing up this year, people will more and more weird songs that they never heard before. Sometimes we don’t like to [perform new material], because people are always recording every doggone thing now. No matter what you do, you look on YouTube and it’s there!
Looking toward the future, I wanna do a gospel album. In my head, I want to do the gospel songs I’ve done with my choir. I always try to rearrange songs, like “Keys to the Kingdom” or “Already Been to the Water.” I can hear the Dap-Kings behind me — I could make up some horn lines! This is how I’m battling cancer and beating this sickness: Just keep working. I don’t wanna sit home and wait for the cancer to take over my body. I’ve gotta keep fighting, taking it one day at a time.
Image of Sharon Jones:(Scott Legato/Getty Images)
Originally Posted By: Eric Renner Brown, EW.com
Cancer.Gov
A new study has found that drinking water from private wells, particularly dug wells established during the first half of the 20th century, may have contributed to the elevated risk of bladder cancer that has been observed in Maine, New Hampshire, and Vermont for over 50 years. Other risk factors for bladder cancer, such as smoking and occupational exposures, did not explain the excess risk in this region. The study, by researchers at the National Cancer Institute (NCI), part of the National Institutes of Health, and colleagues at the Geisel School of Medicine at Dartmouth, Hanover, New Hampshire; the departments of health for Maine, New Hampshire, and Vermont; and the U.S. Geological Survey, appeared May 2, 2016, in the Journal of the National Cancer Institute.
Bladder cancer mortality rates have been elevated in northern New England for over half a century. The incidence of bladder cancer in Maine, New Hampshire, and Vermont has been about 20 percent higher than that in the United States overall. Rates are elevated among both men and women. A unique feature of this region is the high proportion of the population using private wells for their drinking water, which are not maintained by municipalities and are not subject to federal regulations. These wells may contain arsenic, generally at low to moderate levels. Previous studies have shown that consumption of water containing high concentrations of arsenic increases the risk of bladder cancer.
There are two possible sources of arsenic in the well water in northern New England. Arsenic can occur naturally, releasing from rock deep in the earth, and arsenic-based pesticides that were used extensively on crops such as blueberries, apples, and potatoes in the 1920s through the 1950s.
“Arsenic is an established cause of bladder cancer, largely based on observations from earlier studies in highly exposed populations,” said Debra Silverman, Sc.D., chief of the Occupational and Environmental Epidemiology Branch, NCI, and senior author on the study. “However, emerging evidence suggests that low to moderate levels of exposure may also increase risk.”
To explore the reasons for the higher rates of bladder cancer in northern New England, the researchers conducted a large study in Maine, New Hampshire, and Vermont. They compared 1,213 people newly diagnosed with bladder cancer with 1,418 people without bladder cancer who lived in the same geographic areas as those who developed the disease. The researchers obtained information on known and suspected bladder cancer risk factors, including smoking, occupation, ancestry, use of wood-burning stoves, and consumption of various foods.
“Although smoking and employment in high-risk occupations both showed their expected associations with bladder cancer risk in this population, they were similar to those found in other populations,” said Silverman. “This suggests that neither risk factor explains the excess occurrence of bladder cancer in northern New England.”
Researchers estimated the total amount of arsenic each person had ingested through drinking water based on current levels and historical information. They found that increasing cumulative exposure was associated with an increasing risk of bladder cancer. When investigators focused on participants who had used private wells, they saw that people who drank the most water had almost twice the risk of those who drank the least. This association was stronger if dug wells had been used. Dug wells are shallow, less than 50 feet deep, and potentially susceptible to contamination from manmade sources. Most of the dug well use occurred a long time ago, during an era when arsenic concentrations in private well water were largely unknown. However, the risk was substantially higher if the dug well use began before 1960 (when application of arsenic-based pesticides was commonplace in this region) than if dug well use started later.
The major limitation of the study was the inability to precisely measure arsenic exposure in the water consumed by people over their entire lifetime, which made it challenging to accurately quantify the contribution of arsenic exposure to the excess risk of bladder cancer. In particular, there were no known measurement data on arsenic levels in well water in the region prior to the 1960s, when arsenic-based pesticides were in widespread use.
The likelihood of exposure to arsenic from dug wells has diminished in recent years because arsenic-based pesticides are no longer used. Also, dug well use is much less common now than in the past. However, possible current exposure to arsenic in drinking water through use of private wells drilled deeply into fractured bedrock is a potential public health concern. For reference, the U.S. Environmental Protection Agency has established 10 micrograms per liter as the regulatory standard for arsenic in drinking water supplied by municipalities.
“There are effective interventions to lower arsenic concentrations in water,” said Silverman. “New England has active public health education campaigns instructing residents to test their water supply and to install and maintain filters if levels are above the EPA threshold. But we should emphasize that smoking remains the most common and strongest risk factor for bladder cancer, and therefore smoking cessation is the best method for reducing bladder cancer risk.”
ESPN.com news services
The chemotherapy has diminished Craig Sager’s once-lustrous chestnut hair to a few unruly strands, and on this day of hope, a simple green T-shirt and blue shorts adorn the man known by millions for his ostentatious wardrobe and easy rapport with the NBA’s elite.
He methodically extended a long, skinny arm to an IV pole holding the stem cells he is counting on to save his life. There was silence as he cradled the tube, watching the crimson liquid drip, drip, drip in a perfect cadence into the cannula feeding it into his cancer-stricken body.
TNT’s beloved basketball broadcaster received a rare third bone marrow transplant on Wednesday as an aggressive form of leukemia continues to take its toll. Sager, 65, has battled acute myeloid leukemia since 2014 and announced in March that he was no longer in remission.
Sager knows the odds are against him. Yet, he is unfazed.
“I like to gamble,” he told The Associated Press. “I like to bet on horses, I like to bet on dogs. I like to bet on a lot of things. I’ve bet on a lot of things with a lot higher odds than this.”
Two other times, Sager received a bone marrow transplant with stem cells, and in both instances, it put him into remission for several months. His son, Craig Sager II, was the donor then. This time, the anonymous 20-year-old donor was considered a perfect match.
Sager has been hospitalized for a month and has another monthlong stay ahead. He hasn’t thought a lot about the man whose bone marrow could change everything for him. But when he learned of the donor’s age, he expressed a possibly only half-serious concern.
“My only thing was, I was afraid that when he signed up to be the donor, he may have been in some drunk fraternity house, trying to impress his date,” Sager said with a smile. “And they call him up the next day and say, ‘Want to come down to the hospital?’ and he’s like, ‘What?'”
His fears turned out to be unfounded.
“He came through,” Sager said.
It is the latest of close to 100 procedures Sager has endured in his well-publicized fight, and it was performed at MD Anderson Cancer Center in Houston. Sager began the transplant at about 11:30 a.m. CT, and it wasn’t complete until more than 10 hours later.
Dr. Muzaffar Qazilbash, Sager’s stem cell transplantation physician, researched thousands of such transplants at MD Anderson over the past 15 years to illustrate just how uncommon Sager’s procedure was.
“It’s less than 1 percent of the total number of transplants,” Qazilbash said. “It’s very rare to have three transplants.”
As Sager said moments after the process began, “OK, third time’s the charm.”
Sager, who has worked for TNT for more than three decades, calls himself coachable and said he is open to trying anything doctors believe might help.
“I’ve had every chemo in the alphabet, most of them more than once,” he said. “Some of them that aren’t even in the alphabet, they’re just numbers — clinical trials. But I bet if you added all those up, it would have to be like 60- or 70-something. I’ve had 23 bone marrow aspirations. Having one isn’t fun, and I’ve had 23. So that’s been tough.”
Despite the rigors of treatment and how it can ravage his body, he has never thought about giving up. In fact, he gets angry when he meets other patients who say they’ve grown weary of fighting.
“Man, life is too beautiful, too wonderful, there’s just too many things,” he said. “It’s not just you. It’s your family and kids and all. Fight. Fight until the end. Fight as hard as you can.”
With his radiant smile and TV-perfect persona, it takes time to peel back the layers of positivity and catch a glimpse of how hard that fight can be.
“His attitude is [that] nobody wants to hear it,” said Stacy Sager, his wife, full-time caregiver and No. 1 fan. “And so it makes you reflect on yourself and the things that you say when you’re complaining about little things in life and trivial things, and it just puts things in perspective.”
But there are times, often as night creeps into early morning, where it all becomes too much. No medication can help.
“I’ve never had any of those days where I’ve actually said, ‘Why me’ or ‘I can’t do it,'” he said. “But I’ll have some dark nights where I’ll be here by myself and maybe getting some medicine that’s making me jump around like a rabbit. And I’m in pain and I’ve got chills and I’ve got fever and I’ve got everything mixed into one and I’m throwing up and have diarrhea … and I’ll just say, ‘Stacy, I need you. I need you.’
“And she’ll come to me and just hold me, and it just makes it better.”
A few days before his transplant, Stacy came down with a bad cold and doctors sent her home, fearful she would transmit her illness to her husband. Hall of Famer and TNT colleague Charles Barkley heard she couldn’t be there for a couple of days and hopped on a plane from Phoenix.
The problem was that Barkley had hip replacement surgery less than a month ago and wasn’t cleared to travel. He said his doctor was livid when he learned Barkley had defied orders and flown halfway across the country. Barkley informed the doctor that it was an emergency — although it was hard to know who was there for whom.
“Craig Sager is one of the most interesting people I’ve ever met,” Barkley said. “We go to see Sager to cheer him up, and by the time you leave, you’re like, ‘Is anything wrong with him?’ He has the most positive attitude.
“When you go to try and cheer him up, his attitude is so upbeat, he cheers you up.”
Sager has found inspiration in a little girl who lost her fight with cancer before her ninth birthday. He befriended Lacey Holsworth and her family while working on a story about her illness and remained friends with her parents after she died in April 2014. Holsworth had cheered on the Michigan State basketball team and had a close friendship with star player Adreian Payne.
Last weekend, her parents visited Sager in his Houston hospital room. They left him with a more tangible reminder of her bravery.
“They brought me little Lacey’s boots that she used to always wear to games and a picture of her wearing them,” Sager said, clutching the high-top cheetah footwear accessorized with laces made from silk ribbons. “That little girl was so amazing. Fought for all of those years, was always positive, always cheerful, always brought other people’s spirits up. So if I’m laying here feeling bad, I just think about Lacey, and it puts everything in perspective.”
Sager also is bolstered by his drive to be back on the sideline for the NBA season. He doesn’t expect to have recovered from Wednesday’s transplant in time for the season opener Oct. 25 but aims to return by early November for more gentle sparring with the likes of San Antonio Spurs coach Gregg Popovich.
It would be a victory not just for him, but for all the people his fight has inspired
“It means that you’re surviving and you’re winning,” he said. “That you’re knocking down obstacles and clearing hurdles that are put in front of you and you’re doing them with flying colors.”
On Wednesday, five colorful balloons were tied to one side of his hospital bed. Several had birthday greetings and two read: “Happy birthday, it’s your big day.”
Festive, yes. But Sager was born in June.
“When you get stem cells, they say it’s your new birthday,” Stacy explained. “So this is his fourth birthday.”
Sager tried to downplay the pageantry surrounding the event, saying it wasn’t “a big deal.”
That earned a sweet, yet stern, admonishment from his beloved wife.
“It is a big deal,” she said. “It’s giving you life.”
The Associated Press contributed to this report.
Laurie McGinley, The Washington Post
Bald but beaming, 5-year-old Eden Oyelola yanked the long rope to ring the “victory bell” at Children’s National Medical Center last September. She was finally done with her treatment for brain cancer — surgery followed by months of radiation and chemotherapy that made her terribly ill.
At a “bell party” at her home in Upper Marlboro, Md., later that week, she gobbled down ice cream with friends and rode a pony around the back yard. Her parents exhaled in relief. “We thought she was in the clear,” her father said.
The relief was short-lived.
In January, the little girl who loved gymnastics started having seizures and losing control of her left side. She frequently stumbled. “What’s wrong with my legs?” she asked. A second surgery followed after an MRI showed that the tumor had returned, forcing her doctors at Children’s to ask whether there was anything else that would give Eden a chance to survive.
The team ultimately turned to the hottest field in medicine and a new class of drugs that has had stunning success in some adults, including former president Jimmy Carter, with even hard-to-treat malignancies. Growing ranks of pediatric oncologists are considering immunotherapy and “checkpoint inhibitors” to try to save desperately ill children.
But young patients with cancer present a special challenge. Research can seem more dangerous because of their age, and drugs that work in adults may fail for the same reason. No one can yet say with certainty whether — or to what degree — these treatments hold equal promise for children.
That allows for hope as well as, in Eden’s case, devastating disappointment.
“It’s a new horizon that we need to explore and see if it can help these kids,” said Brian Rood, Eden’s neuro-oncologist. “But we’re still learning how to use it.”
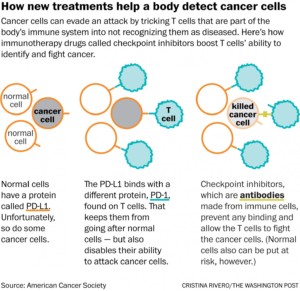
Immunotherapy, which one specialist calls “the fourth pillar of cancer treatment” after surgery, radiation and chemo, marshals the body’s immune system to fight a malignancy. As part of that approach, checkpoint inhibitors disrupt a cloaking device tumors wield to evade and suppress T cells, the foot soldiers of the immune system. Once T cells can see the cancer, they attack it just as they would other foreign intruders such as bacteria.
Four checkpoint inhibitors have been approved for adults, but they are only now undergoing broader testing in children. The lag reflects the many significant hurdles of conducting clinical trials with this age group.
Eden’s doctors set their hopes on a first-of-its-kind clinical trial led by Children’s, a study testing a checkpoint inhibitor treatment in children who have aggressive brain tumors. The complex strategy has its own set of risks; the treatment often causes inflammation and swelling, a dangerous combination in the contained space of the brain.
n describing the trial to Eden’s parents, Rood was cautious. Their daughter would need yet another surgery to reduce the size of her tumor, and there was no guarantee she would be eligible for the trial after that, or that the treatment would work.
“About the best we can say,” Rood acknowledged, “is that we don’t know that it doesn’t work.”
“Eden will be a guinea pig,” thought Eden’s mother, Sara Amare. But like her husband, Toks Oyelola, she was eager to press ahead. Both knew that the study medication, Keytruda, also called pembrolizumab, was the same one that Carter received after advanced melanoma spread to his liver and brain. Last December, following surgery, radiation and the immunotherapy, the former president announced that his cancer had disappeared.
“He was 91,” Amare said. “I thought, ‘Surely, this will work in a 6-year-old.’ ”
As a child with cancer, Eden belongs to a relatively small group. An estimated 16,000 children up to age 19 will be diagnosed with the disease in the United States this year, and it will kill fewer than 2,000. By contrast, about 1.6 million adults are expected to get a diagnosis, and more than 590,000 will die of the disease.
Pediatric oncologists complain that medicines for children are too few and too toxic, largely because drug companies focus their efforts on the adult market. Only one immunotherapy drug has been specifically approved for pediatric cancer.
“Over the last 30 years, we have had very, very few new drugs in our clinics, and we still rely on radiation and chemo,” said Michael Jensen, director of the Ben Towne Center for Childhood Cancer Research at Seattle Children’s. “When a drug is developed for prostate cancer or breast cancer or colon cancer, they will say, ‘Here, try this for kids with brain tumors.’ It really doesn’t help these underserved kids.”
Researchers have long known that children are not simply miniature adults; they are biologically different. They tend to get different cancers than adults — leukemia rather than lung cancer, for example — and even the same cancer can play out differently in their bodies.
So, perhaps, may immunotherapy. Many adult tumors have mutations caused by cigarette smoke, sunlight and other environmental insults. Once unmasked by a checkpoint inhibitor, such mutations can be seen by the immune system as “foreign” and deserving of attack. Children’s cancers, however, generally have far fewer mutations and thus may offer fewer targets, according to one theory.
Another kind of immunotherapy, called CAR-T cell therapy, is being widely tested in children with acute lymphoblastic leukemia, the most common and once universally fatal childhood cancer. It has shown extraordinary effectiveness in treating recurrent disease.
By contrast, checkpoint inhibitors in children “may not be the home run they are in adults,” said Crystal Mackall, head of the cancer immunology and immunotherapy program at the Stanford University School of Medicine. “But it’s too early to know.”
The Oyelola family lives in a comfortable house in Prince George’s County, with a back yard big enough to accommodate pony rides on special occasions. Eden, who is obsessed with unicorns, has a 7-year-old sister, Sade, and an 18-month-old brother, Tobi.
“He chases me, then I chase him,” Eden said on a recent afternoon as the children raced around. Dressed in a shirt decorated with lions, tigers and zebras, she showed little sign of being sick, other than a little puffiness in her face and slightly shorter hair where she had surgery.
 Eden and her sister Sade (Michael S. Williamson/The Washington Post)
Eden and her sister Sade (Michael S. Williamson/The Washington Post)
Eden’s father is a consultant for Ernst & Young whose parents came from Nigeria decades ago. Her mother is a native of Ethiopia who moved to the United States as a little girl. A wall of photographs in the family room shows a handsome and happy family.
On Halloween 2014, Oyelola remembers, “a new normal” took hold. Amare was driving their daughters home from a school parade — Eden had been dressed up as the country of Russia. Suddenly, Sade cried from the back seat: “Mommy, Eden is shaking!” Saliva foamed on her lips.
Doctors at Children’s diagnosed a febrile seizure, a not-uncommon event in childhood. But several weeks later, another seizure followed. This time, Children’s did a scan. “We see a mass,” the doctors told Amare. Brain surgery was scheduled for Christmas Eve.
Eden’s family decorated her intensive-care room with lights, wreaths and a tree. When she woke up on Christmas, she was amazed by the presents, sneaked in by nurses, and by a visit from Santa Claus himself.
Those would be the only bright spots of the holiday.
The ultimate diagnosis was that Eden had a “primitive, very rare, very unusual tumor,” Rood said, with many of the characteristics of glioblastoma. This deadly type of cancer arises from glia cells, which support brain function.
Months of radiation and chemo followed, ending with the bell party in September 2015. Late last year, the Make-A-Wish Foundation arranged for the family to go on an all-day scavenger hunt that culminated in a ride on a “unicorn” at Verizon Center. “Yes, it’s a real unicorn!” Eden declared, caressing the big white horse.
The tumor’s return in January was a crushing blow. Eden quickly had surgery and eventually entered a clinical study involving pomalidomide, a thalidomide derivative that is thought to interfere with tumor growth. She began getting violent headaches. “She could wake up in the morning and be hysterical for two hours,” her father said. And she was having three to four seizures an hour.
The doctors took her off the medicine and talked to her parents about the immunotherapy trial and another operation. “It was nerve-racking,” Rood said. Yet they had no other options.
In late May, Eden had her third surgery, which succeeded in sharply reducing the tumor and the swelling, and in easing her pain. A few days later, she celebrated her sixth birthday.
Not long after, she got a spot in the Children’s trial.
Brain and central-nervous-system tumors are the second-most-common type of childhood cancers, after leukemia. A patient’s prognosis depends on the type of malignancy, whether cancer cells remain after surgery and whether the tumor recurs.
Given the success seen with checkpoint inhibitors for some adult cancers, there is intense interest in trying them in brain tumors in patients of all ages. The hope is that the immune system will be effective at attacking the tumor and breaching the blood-brain barrier, a kind of security system that protects the brain yet also prevents many treatments from getting through.
Several pediatric trials are underway or in development, including one trying a combination of checkpoint inhibitors that New York’s Memorial Sloan Kettering Cancer Center has set for next year.
The safety-and-feasibility trial at Children’s and other institutions is co-sponsored by the National Cancer Institute and the Pediatric Brain Tumor Consortium, a network of children’s hospitals and academic medical centers that conducts early-stage studies of novel treatments. Up to 70 patients will be enrolled, ages 1 to 21, with participants given infusions of Keytruda for 30 minutes every three weeks. The treatments are slated to extend over two years.
Eugene Hwang, a pediatric neuro-oncologist at Children’s, and the other investigators are proceeding carefully because of the risks, frequently “pausing” the study to examine results and decide whether changes are needed. One of the toughest challenges in using checkpoint inhibitors or any immunotherapy for brain tumors, Hwang said, is figuring out how to produce the right level of immune response. Too weak and it won’t affect the tumor. But too strong and the swarm of T cells could trigger lethal swelling.
“I have desperation in my back yard, where kids are dying, and there’s hope the next yard over, where adults who have failed trial after trial are surviving,” said Hwang, the study chairman. “There is nothing that is going to dissuade me from trying something that has really revolutionized care for many adults.”
Eden got her first dose of Keytruda on June 22, and everything seemed fine for the first two weeks. But shortly before her planned second dose, she again began having headaches, and numbness in her left arm. An MRI showed that the mass in her head had doubled in size in barely a month.
That raised a critical issue for her physicians: Did the larger mass mean the drug had triggered the robust immune response they wanted? Or was the treatment failing and the cancer’s growth accelerating? Or some combination of both?
It was impossible to tell from the scan. Yet the answer would determine whether Eden could continue in the trial.
The doctors delayed the second dose and gave her steroids to reduce the brain swelling. That effectively negated the effects of the immunotherapy, but it was the only way to figure out what was happening as they chose how to proceed.
Her family tried to carry on with life. They all took a vacation to the beach, making sure they visited Assateague Island to see the wild ponies.
Eden seemed to be doing well, and her parents were increasingly sure she would soon get her second Keytruda dose. But on July 28, she awoke in intense pain and was rushed the 20 miles to Children’s. The tumor had gotten significantly bigger in just a few weeks and was starting to push the brain from the right side of her head toward the left. Blood and fluid also appeared to be leaking into the space between the brain and the skull.
Doctors treated Eden with high levels of painkillers and higher levels of steroids. And they sat down with her parents. Rood told them that the tumor’s fast growth was making it impossible for Eden to stay on the trial.
Take her home, Rood suggested, and make her as comfortable as possible.
“I can’t accept that,” Amare said later, even as she talked about going “the God route.” At her request, pastors from her Ethiopian Orthodox church have come to pray for her daughter.
Her husband is similarly torn. The doctors, he said, “don’t expect a miracle to happen. But I do.”
Eden still romps through the house and plays with her dogs, Winter and Summer. On a recent afternoon, bored for the moment, she climbed onto her father’s lap and whispered in his ear to take her to Target.
She wanted to get more Twozies to add to her already sizable collection of the toy babies and pets.
“Okay,” Oyelola said with a smile. “Let’s go.”
Photo of Eden Oyelola: Michael S. Williamson/The Washington Post
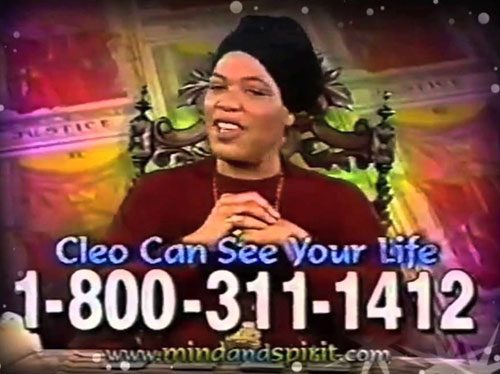
Stalwart of late-night commercials of the late ’90s and pop culture touchstone “Miss Cleo” died Tuesday after a battle with colon cancer, her lawyer confirmed to the Associated Press. She was 53.
A “pillar of strength” throughout her illness, which eventually spread to her liver and lungs, Cleo died surrounded by family and friends, her representative told TMZ, which first reported the death. Harris’ lawyer, William J. Cone Jr., confirmed the death to AP.
Born Youree Harris in Los Angeles in 1962, Cleo became a cultural icon as the spokeswoman for Psychic Readers Network, where she starred in infomercials as a Jamaican psychic, replete with accent, who used tarot card readings to advise individuals who used the pay-per-call service on their futures.
Her success was cut short when, in the early 90s, lawsuits against the network began cropping up in states across the country alleging fraud. The Federal Trade Commission charged the company’s owners with deceptive advertising, billing and collection practices in 2002. Though Cleo was not charged, it was revealed at that time that she was born in Los Angeles to American parents.
Originally posted By: Libby Hill on latimes.com
Originally posted by: Felix Gussone, MD on nbcnews.com
The number of cancers related to HPV has dramatically increased, a new government report finds. But too few people are receiving the best protection against the preventable and potentially deadly diseases of the cervix, head and neck: a vaccine given to pre-teens which could protect them later in life.
The number of human papilloma virus (HPV)-associated cancers in the United States has increased by 17 percent, to nearly 39,000 cases a year, according a report released Thursday from the Centers for Disease Control and Prevention.
While men cannot get HPV-linked cervical cancers, they are particularly vulnerable to HPV-related cancers of the mouth, tongue and throat, called oropharyngeal cancers. According to the new CDC report, the rates of mouth and throat cancers are more than four times higher among males than females.
“In the past, people always felt that the boys needed to be vaccinated to protect the girls but, truthfully, they need to be vaccinated to protect themselves”, says Dr. Lois Ramondetta , professor of gynecologic oncology at MD Anderson Cancer Center who has made it a personal mission to educate both parents and pediatricians about HPV and the vaccine that can help stop cancer before it starts.
Ever since actor Michael Douglas announced in 2013 that he suffered from HPV-related throat cancer in 2013, people realized HPV poses a threat not only to women, but to males of all ages.
“There is an epidemic of HPV related cancers in men, specifically those of the tonsil and the back of the tongue,” says Ramondetta. “What’s really important to know about those is that there is no screening test for those.”
A recent study in the Journal of the American Medical Association found that HPV infection raises the chances of throat, mouth or tongue cancer by at least sevenfold. Experts predict that throat cancer will beat out cervical cancer as the most common HPV-related cancer by 2020.
The most effective way to prevent that: Early vaccination.
Boys and girls are supposed to get three doses of the HPV vaccine — starting at age 11 or 12 because the vaccine works best before sexual activity begins.
“The other benefit of giving it early is that our immune response is better. And that it may last longer,” Ramondetta explains.
Yet the latest statistic from the CDC shows that in 2014, only 40 percent of teenage girls received all three doses of the vaccine needed. In boys, that number is even lower: Only 22 percent of boys between 13 and 17 are properly vaccinated against HPV, increasing their chances for HPV-caused cancers later in life.
“We actually know the majority of them can be prevented with the HPV9 vaccine that’s out now,” says Ramondetta. In fact, the new CDC study found that 93 percent of all HPV-caused cancers are preventable with existing HPV vaccines.
According to the CDC, the HPV vaccine — which is usually covered by insurance — is safe and not associated with serious side-effects of the HPV
Originally posted by: Amanda Jackson, CNN.com
A Washington woman is praising her daily snack for helping her discover a cancerous tumor.
Kristine Moore says she has been eating Ruffles potato chips for the last 20 years. The Marysville, Washington, resident packs them for lunch every day. In February, while she was munching on her faithful snack, she felt a sharp pain as a chip poked the back of her throat.
She asked her husband to look inside her mouth. “He said, boy, your tonsil looks very red and swollen,” Moore told CNN affiliate KIRO.
The next day, she went to the doctor, suspecting that she was coming down with a cold. However, after a test for strep throat came back negative, her doctor decided to biopsy the swollen tonsil. Moore had throat cancer.
“It’s called squamous cell carcinoma on my left tonsil,” Moore said.
In 2015, about 39,000 people in the United States were diagnosed with throat cancer, according to the American Cancer Society. Depending on the type of cancer, treatments can entail surgery, radiation and chemotherapy.
Squamous cell carcinoma has a strong correlation to tobacco use. Moore said she was a smoker for years before quitting shortly after her diagnosis.
In 2010, legendary NBA coach George Karl was diagnosed with the same cancer on his right tonsil. He recovered and continued coaching. But for film critic Roger Ebert, who was also diagnosed with head and neck cancer, the outcome was different. Ebert suffered complications from surgery that left him disfigured and without the ability to speak. He passed away in 2013.
For Moore, her outcome is more positive. Her doctors said her cancer was caught early. Now she will begin radiation and chemotherapy treatment.
“The potato chip was a blessing in disguise,” Moore said. “I probably wouldn’t have found out another year.”
Potato chips are not an at-home cancer test by any means or even a healthy snack. A trip to the doctor for an annual check up could have caught this cancer as well.